Introduction
You’re already familiar with some rules of thumb for avoiding COVID-19 infection: wear a mask, stay 6 feet apart (or 2 meters, depending on where you live), and only socialize outdoors. But is it riskier to go to the grocery store, or to ride in a Lyft or Uber? It’s tough to make good choices when you don’t know how large or small the risks really are.
We, the authors, were really struggling with this. We wanted a better way to make decisions about COVID risk. So we read some papers and crunched some numbers. We spent hours building a model to estimate the COVID risk of various activities. And in this writeup, we’ll share our model (and some practical tools!) with you.
We’ll show you:
- how we estimate COVID infection risk, in units of “microCOVIDs”
- how risky we think various common activities are
- how you can estimate the COVID risk of your own actions (by hand, or using our handy-dandy calculator)
- and, most importantly, how to make decisions that balance living your life with safety and health.
You’re in the target audience of this white paper if you are comfortable with numbers and want to think about how your personal choices affect your chance of getting COVID-19. We are not focusing on society-wide pandemic dynamics, policy responses, or suggestions for public health officials.
How to navigate this white paper
Use the “previous” and “next” links at the top or bottom of the page to navigate from one section to the next.
Footnotes[1] usually contain nerdy details for detail-loving readers, and often a link to even more gory detail in the Research Sources section.
Disclaimer
We have based our numbers in this writeup on published scientific research. However, unlike a medical or scientific standard of evidence, we state our best guess based on available evidence, even when that evidence is far from conclusive. Our goal in doing so is to enable ordinary people to do back-of-the-envelope calculations to make personal decisions. For scientific data, please see the Research Sources that we have used in forming our guesses.
We have read a lot of experts' research, but we are not ourselves experts in this topic. This is not a primary source of new information about COVID. This work has not been scientifically peer-reviewed. There is still a lot of uncertainty about COVID. Do not rely on this tool for medical advice. Please continue to follow government guidance.
Authors:
This article (and corresponding calculator) was originally collaboratively written by the members and friends of Ibasho, a communal house in San Francisco. Our goal is to protect our broader community’s physical and mental health during the pandemic, by promoting balanced evidence-based decision-making by individuals in our community.
Since then, the project has grown to include like-minded individuals around the world.
Cite us collectively as: The microCOVID Project
Original White Paper and Model: Catherine Olsson, Joshua Oreman, Rhys Lindmark, Anna Tsykalova, Stephanie Bachar, Sarah Dobro, MD, Matt Bell
Website and calculator: Dominic Dagradi, Sarah Dobro, Ben Shaya, Deb Lyon, Jeremy Blanchard, Matt Bell, Jenny Wong, Melody Chang, Josh Oreman, Peter Gyongyosi, Michael Cohn, Justin Haaheim, Vince Broz and the microCOVID GitHub community.
Ongoing Model Researchers: Catherine Olsson, Ben Shaya, Joshua Oreman, Riley Drake, Alanna Slocum
Risk Tracker: Jeremy Blanchard, Catherine Olsson, Joshua Oreman, Ben Shaya
Social Media and Blogging: Catherine Olsson, Ben Shaya, Matt Bell, Luke Lew, Finan Adamson
Feedback & assistance thanks to: Ajeya Cotra, Andrew Critch, Andy Matuschak, Danny Hernandez, David Mears, Derek Foster, Elliot Olds, Eugene Shvarts, Jacob Falkovich, Jeremy Howard, Jessica Watson Miller, Ivan Gayton, Katja Grace, Matt Bell, Peter Favaloro, Peter Hurford, Zvi Mowshowitz, and other friends who chose to remain anonymous. (Giving feedback does not imply endorsement of, or agreement with, this writeup.)
Throughout the text, you will see footnotes like this. Usually they will have some content, but this one is just a demo! You can click the arrow to return to where you came from in the text: ↩︎
We measure the riskiness of interactions in “microCOVIDs”
You might have seen images categorizing COVID risk as “high,” “medium,” or “low” or rating activities on a riskiness scale from 1 through 9. This is helpful, but personally we found that we had to dig further—into actual numbers—so we could make confident decisions.
Calling an event “high risk” is like categorizing a furniture purchase as “expensive.” If I’m buying a rug, and I know it’s “expensive,” but it would really complete the look of my room, can I afford to splurge this time? Maybe, or maybe not! If the rug is $100, that might be a sensible purchase. But if the rug is $10,000 then I might have difficulty paying for rent and groceries if I buy it!
Similarly: if I’ve been told that going to gatherings is “high risk” but I really truly miss my friends and there’s a picnic coming up I want to attend, should I go? Is this high risk like skiing, or high risk like jumping off a cliff?
We would like to give you a research-based, quantitative framework to answer questions like these.
We can use research to numerically estimate COVID risk
Some people might not realize that it’s even possible to measure and numerically quantify the risk of getting COVID. Most sources tend to give non-quantitative advice, such as “the CDC recommends that everyone wear a mask to reduce transmission.” This advice is good, but we would like to go even further.
Fortunately, there are now many research papers available about the numerical likelihood of getting COVID from different kinds of interactions. You can search for these studies on Google Scholar and read them yourself. Some of these studies are not peer-reviewed (which is the gold standard for scientific publication), so it’s extra important to analyze them carefully. While none of us are public health experts, we have enough academic background to feel comfortable wading into the literature to come up with numerical estimates. We explain more of our reasoning in footnotes and in the Research Sources section.
Measuring COVID risk in “microCOVIDs”
So let’s get started. To quantify the risk of an individual interaction—say, meeting a friend for coffee—we’re going to think in terms of microCOVIDs (abbreviated μCoV)[1]: a one-in-a-million chance of getting COVID[2].
1 microCOVID = a one-in-a-million chance of getting COVID
For example, if you live in a region where about 1 in 1,000 people currently has COVID, then you could calculate based on studies of other indoor interactions (as we will explain later in this writeup) that meeting a friend for coffee indoors has about a 1 in 17,000 chance of giving you COVID. Such small numbers are hard to think about, so we can use microCOVIDs instead. Your coffee date would be about 60 microCOVIDs. By the end of this white paper, you will understand how to do these calculations yourself.
One benefit of using microCOVIDs is that you can straightforwardly add up microCOVIDs to estimate your risk over longer periods of time.[3]
- Here’s an example (using some made-up numbers): last week you made two trips to the grocery store (25 microCOVIDs each), went for two masked outdoor walks with friends (1 microCOVID each), and otherwise stayed home alone, so your total risk for that week would be 52 microCOVIDs. You can imagine doing the same calculation over longer time intervals to estimate your chance of getting COVID in a month or even a year of activities.
We use microCOVIDs rather than some other scale factor (milliCOVIDs? nanoCOVIDs?) because they tend to come out as conveniently-sized numbers.
How much is a microCOVID?
This whitepaper was started by a group of 30-something-year-olds in San Francisco who live together in a communal 9-person house and mostly work from home. After much discussion (which we hope to explain later in a future post), the household agreed to aim to keep each housemate's individual risks of getting COVID below 1% per year[4] (i.e., about 10,000 microCOVIDs per year). Important factors in this decision were that nobody in the household regularly interacted with anyone who was at high risk of severe illness from COVID, and that the household collectively cared a lot about doing their part to reduce the spread of the pandemic.
Each person had 2,400 microCOVIDs to spend per year after taking into account how many microCOVIDs would be used up just by living with each other[5]. With this budget:
| An activity that measures this many microCOVIDs... | feels this risky… | … and we could do the activity this often, if we were not doing much else |
|---|---|---|
| 1 μCoV | almost negligible | dozens of times per week |
| 10 μCoV | moderate risk | a few times per week |
| 100 μCoV | quite substantial risk | once or twice a month |
| 1000 μCoV | borderline reckless | once a year, maybe |
Choosing your risk budget
In general, if you are young and healthy, don’t regularly visit anyone who is older or has COVID risk factors, and are lucky enough to be able to make voluntary choices about your risk exposure, then we think aiming for 10,000 microCOVIDs per year (corresponding to 1% risk of COVID per year) is a plausible choice.
You can read more details on choosing your risk budget here.
What we want you to take away from this section is that for people under 40, an activity that is 1 microCOVID is very low risk, whereas an activity that is 1,000 microCOVIDs is very high risk. Furthermore, any risk of infection that you incur is not just a risk to you, but also a risk to vulnerable people in your community.
Let’s now explore how to quantify the risk of various activities in terms of microCOVIDs.
μ is the standard abbreviation for “micro,” the unit prefix meaning “one millionth.” For example, one microgram (μg) is one millionth of a gram. ↩︎
Strictly speaking there is a difference between “getting SARS-CoV-2” (the virus itself) and “getting COVID-19” (the disease caused by the virus). In the rest of this article, no matter what language we use, we are talking about the total chance of getting infected, including if you show no symptoms and are an asymptomatic carrier of the virus. We chose to use “microCOVIDs” (referring to the disease) instead of “microCoV” (referring to the virus) for this article based on reader feedback that it was simpler and easier to understand. But we emphasize that we are not excluding asymptomatic infections from this measurement. ↩︎
Technical note—skip if you’re not interested in the underlying math! If you’ve worked with probabilities before, you might worry that adding them together like this is too straightforward to possibly be correct. There’s an underlying nonlinearity: while you could accumulate well over a million microCOVIDs if you do enough risky things, your chance of getting COVID can never be higher than 100%. To properly compute the probability that you remain uninfected despite independent activities A and B, you should calculate
”probability not infected via A” * “probability not infected via B”. If you’d prefer to add instead of multiplying, then you’ll need to take a logarithm somewhere. Thus, to be fully correct, the formula for converting a risk (like 0.01 or 1%) to microCOVIDs should be-1,000,000 * ln(1 - risk). You can use calculus to verify that when the risk is small, this is very well approximated by the simpler1,000,000 * risk. For values as high as 100,000 microCOVIDs, the error introduced by ignoring the logarithm is still within about 5%. The uncertainty in our other estimates is at least that large, so we think the simplification is reasonable. For calculations involving a multiple interractions with substatial risk (any calculation tha would result in >10% chance of infection), the calculator switches to multiplying for accuracy. ↩︎Technically, what we mean when we say “1% per year” is a 1% annualized risk. That is, if we go 6 months without getting sick, we aren’t going to double our chances and bump up to a 2% chance in the following 6 months to even it out. We’ll continue at the same 1% annualized risk level. ↩︎
We have a detailed write up on how to adjust your budget given the number of people in your household/pod. ↩︎
Understanding COVID transmission
First, let’s strengthen our intuitive model of COVID transmission.
COVID is transmitted primarily through tiny droplets produced when an infected person talks, coughs, or sneezes (CDC FAQ), many of which can remain suspended in the air for minutes to hours. Touching contaminated surfaces or objects is possibly a way that COVID spreads, but the CDC believes the main way it spreads is person-to-person through respiratory droplets. Therefore, in this writeup, we focus primarily on the risk from exhaled droplets in the air.[1]
To visualize how exhaled droplets work, we suggest a helpful metaphor from our friend Matt Bell. Think of everyone around you exhaling cigarette smoke. If someone is smoking a cigarette in a park 30 feet (10 meters) away from you, you might not even smell it. But in a crowded bar where indoor smoking is permitted, the air will be thick with people’s smoky exhalations.
If you inhale just a bit of “smoke” (exhaled air) from someone with COVID, you might be fine. But if you inhale lots of “smoke,” you’re likely to get COVID. If you’re wondering about the riskiness of a situation, then it’s helpful to imagine, “What if everyone here were smoking a cigarette? How much smoke would I breathe in?” If you’d be breathing in other people’s smoke, then it’s a risky situation.

With enough technology, we can see this "smoke" and see how masks reduce it. Source: https://www.lavision.de/en/news/2020/4302/
Concretely, this means it’s important to avoid situations that feature the 3 C’s: Crowds, Closed Spaces, and Close Contact. Why? Because if anyone there has COVID, which becomes likelier as the size of the crowd increases, their “smoke” will be blown into your face. Even if you’re not standing near them, it will build up in the enclosed space, making it more likely that you’ll inhale it.
"MOD" hangouts: Masked, Outdoors, Distance
So we know what to avoid: the 3 C’s. But besides staying in our homes, what should we do? We can choose to have “MOD” hangouts: 1-on-1 or small-group socializing that is Masked, Outdoors, and Distanced. These hangouts are MODified from normal. The COVID “smoke” gets stopped by your mask, falls to the ground before it reaches the other person, and dissipates into the air. MODified hangouts are much safer, especially when they don’t involve many people.
Later in this document, we’ll try to answer questions like: How much does a mask actually help? Is it safer to be indoors with a mask, or outdoors without one? Should you stay 6 feet (2 meters) away or 10 feet (3 meters)?
In order to answer these questions with microCOVID numbers (not just “high” or “low” risk), we’ll now dive into the research. You can also skip right to the calculator to start playing with numbers if you prefer.
If you’re worried about surfaces, the best thing to do is to be careful not to touch your face (mouth, nose, or eyes) when out and about, unless you’ve just washed or sanitized your hands thoroughly. Getting the virus on your hands isn’t harmful in itself; it has to get to your mucous membranes in order to infect you. ↩︎
Computing microCOVIDs
In order to calculate the actual risk of an activity in microCOVIDs, we need to combine two numbers:
- Activity Risk: the chance that this activity will transmit COVID to you, if the other person currently has COVID.
- Person Risk: the chance that the other person currently has COVID. This is based on overall prevalence in your area and their recent behaviors.
For example:
- Let’s say you do an activity with someone (like watching a movie indoors) that has an 8% chance of transmitting COVID to you if they currently have COVID. We call that an Activity Risk of 8%.
- And let’s say that person has a 1% chance of currently being COVID-positive. We call that a Person Risk of 10,000.
- Just like for microCOVIDs, if someone has a one-in-a-million chance of having COVID, we’ll say their Person Risk is 1.
- Then your chance of contracting COVID from that activity-and-person pair is
8% x 10,000 = 800microCOVIDs (which is the same thing as0.08%).
In other words, whenever you’re deciding to do an activity, ask:
- How risky is the activity itself?
- How risky is the person you’re doing it with?
We’ll think about our actions in terms of how much they “cost” us in microCOVIDs:
Cost = Activity Risk ⨉ Person Risk
Note that the Activity Risk does not factor in the prevalence of COVID in your area. Nor does it take into account the recent behaviors of the person you are interacting with. It is just about the activity itself, specifically how risky it would be if the person currently had COVID.
The Person Risk is the part of the calculation that takes into account the prevalence of COVID in your area, and the other person’s recent behaviors, such as whether they have behaved in a lower-risk or higher-risk manner recently.
Let’s explore how you can estimate these two numbers (Activity Risk and Person Risk) for an activity you’d like to do.
Activity Risk
Activity Risk is the chance that an activity will transmit COVID to you, assuming the other person currently has COVID.
In this section we explain how we estimate Activity Risk for an activity involving one other person. If you just want to compare our risk estimates of specific activities (such as grocery shopping for an hour, or eating in a restaurant), and you are not interested in learning how to do those calculations yourself, you could skip this section and instead explore the example scenarios in the calculator.
Our estimate starts with indoor unmasked conversation
We start by first estimating the risk of interacting with a single COVID-positive person indoors for 1 hour at a normal socializing distance of 3 feet (1 meter) while having a normal-volume conversation.
Activity Risk of talking to 1 person who has COVID, for 1 hour, indoors, unmasked, at 3 feet (1 meter) = 14%
So if you have a friend over to your house to chat for an hour, and your friend turns out to have COVID, we estimate the chance of you getting COVID from that single interaction as 14%.
How did we come up with this number? It's a rough estimate combining many sources: the Hu et al. train passenger study, the Jimenez Aerosol Transmission Model, Bi et al. which uses contact tracing data, the Chu et al. meta-analysis, and the Cheng et al. prospective study. We have since increased this number by 1.5x based on a study by Davies et al on the increased contagiousness of B.1.1.7., and then again by another 1.5x based on a study of the Delta variant by Allen et al.. For the gory details of how we combine these sources, please see Research Sources.
Think of this as our “reference interaction.” We can now use it as a starting point to estimate the risk of other kinds of interactions.
Modifiers: duration, masks, location, distance, volume
Not all interactions are exactly an hour, at a distance of 3 feet (1 meter), etc.
To estimate the Activity Risk of a different interaction (an outdoor picnic, or being in a restaurant), we modify our estimate based on how the interaction in question is different from the “reference interaction” above, based on the following factors:
- duration of interaction
- masks
- location (outdoor vs. indoor)
- distance from each other, and
- volume of conversation.
For example, we might consider having lunch with a friend in the park as interacting for 2 hours (duration), outdoors (location), with someone who is sitting about 6 feet (2 meters) away (distance), without masks because you are eating, talking at a normal volume.
Or we might think of a trip to the grocery store as interacting for 30 minutes (duration), indoors (location), with people who are more than 6 feet (2 meters) away most of the time (distance), who are wearing masks, and who are not talking.
Here are our estimates for the change in risk based on these modifiers:
| Modification | Change in COVID risk to me | Citations: Why do we think this? |
|---|---|---|
| I’m wearing a surgical mask[1] | / 2 | |
| Other person is wearing a surgical mask | / 4 | |
| Outdoors | / 20 or more | |
| 6+ feet (2+ meters) distance | / 2 | |
| Each additional 3 feet (1 meter) of distance (up to 12 feet (4 meters)) | / 2 | |
| Loud talking (shouting, talking over music, singing) | ⨉ 5 | |
| Not talking (such as riding the train) | / 5 |
If you’re taking multiple precautions, multiply the COVID risk reductions together. So if you’re wearing a mask and they’re wearing a mask, then your reduction in COVID risk is 2x * 4x = 8x.
What about if the interaction is with more than one other person? We’ll get to this later, in the section on Putting it all together. For now, even though it may seem a little silly, we will still imagine there is just one other person (a picnic with one friend, just one other person in the restaurant, etc).
There are plenty of other precautions you can take to reduce your risk that we don’t describe here. For more on other precautions, see the Q&A.
There is substantial uncertainty in many of these numbers. We’ve taken uncertainty into account when giving our estimates, so that even if we’re off the mark it’s unlikely to expose you to much more risk than you’re comfortable with. We've also used a slightly conservative prevalence estimate, so that our overall estimates are conservative without distorting the relative risk comparisons. See the discussion of Research Sources for details about the data we based these numbers on.
Example calculations
To calculate the Activity Risk of lunch in the park with your friend, start with 14% (the Activity Risk for our “reference interaction”) and apply modifiers as needed: 14% * 2 (hours) / 20 (outdoors) / 2 (distance of 6-9 feet (2-3 meters)) = 0.7%. You have a 0.7% chance of getting COVID from this single activity if the other person has COVID. Note that there is no modifier for masks or volume because the reference interaction is already unmasked and at normal volume.
What about indoor dining with that friend? You’re there for 2 hours, indoors, at a distance of about 3 feet (1 meter), without masks. Start the same way with 14% and apply modifiers: 14% * 2 (hours) = 28%. Since the reference interaction is already indoors, at a distance of about 3 feet (1 meter), without masks, and at normal volume, you don’t need further modifiers. You have a 28% chance of getting COVID from your indoor lunch if your friend has COVID.
Compare the risk of getting sick from these interactions: 28% for indoor dining vs. 0.7% for lunch in the park. That’s a big difference! Remember, your friend won’t necessarily know that they have COVID, and it’s very common to be infectious before you show symptoms. And that’s with only one person!
Hopefully this puts the risk of indoor gatherings into perspective. To compare the Activity Risk of other activities, such as going grocery shopping or attending a large outdoor party, try our calculator or check out the Q&A for tips and tricks. In the next section, we will look at calculating the risk of activities with multiple people.
Masked, outdoor, distanced interactions are much lower risk
Indoor unmasked interactions are quite risky, but being outdoors and wearing masks both make a huge difference.
Masks: We estimate that masks reduce your risk by 8x. This is if both people are wearing masks. Your mask decreases the risk to you by about 2x. And their mask decreases risk to you by 4x. This assumes a reasonably well-fitting surgical mask. For more protection, there are other types of masks you can wear (addressed in the Q&A). Bandanas, buffs, or other single-layer coverings provide significantly less protection than we estimate here (see Research Sources), so for simplicity we treat them as "no mask", even though we do believe they provide some benefit.
Outdoors: We estimate that being outside reduces your risk by 20x or more because the outdoors is well-ventilated, so small respiratory droplets are less likely to accumulate. With any wind, the risk is even less. We think being outdoors is by far the most valuable thing you can do for your safety, although even that is not a guarantee.
Distance seems to be not quite as beneficial as wearing a mask or being outdoors. We estimate keeping 6 feet (2 meters) apart reduces your risk by 2x, and another 2x for each additional 3 feet (1 meter), up to 12 feet (4 meters). This gives a total risk reduction of:
- 2x if you’re 6-9 feet (2-3 meters) away
- 4x if you’re 9-12 feet (3-4 meters) away
- 8x if you’re >12 feet (>4 meters) away
If you’re outdoors and 20 feet (7 meters) away from a person, you can probably ignore the risk from them.
Volume of conversation also matters. If the other person isn't talking, we estimate that reduces the risk to you by about 5x, because they are not expelling as many respiratory droplets. This actually makes some activities where people don't talk much, such as taking public transportation, safer than they would otherwise be. On the other hand, we estimate that loud talking, shouting, or singing increases the risk by about 5x (as compared to a conversation at normal volume) because more respiratory droplets are exhaled and expelled when you are speaking or breathing forcefully.
Curious how we got these numbers? Again, check out the Research Sources!
Household members and spouses/partners are estimated differently
We do the calculation differently for household members and spouses/partners because you’re likely to interact with them on a recurring basis. We estimate a single, fixed Activity Risk for one week of living in the same household as someone who is COVID-positive.
Activity Risk of living with 1 household member, who has COVID, for 1 week = 40%
Activity Risk of living with 1 spouse/partner, who has COVID, for 1 week = 60%
These numbers clearly show that if your housemate gets COVID, it is not inevitable that you will get COVID too! Even if your spouse or partner (who you are likely to share a bed with) gets COVID, your chance of getting it is still only about 60%.
You might ask: why isn’t the risk of getting COVID from someone in your house higher? Why is the estimate of household member risk (40%) only as bad as about 3 hours of hanging out indoors with a friend (at 14% per hour)? We don't really know why this is, but we do know that over the last year and a half, studies continued to find transmission rates within a household well below 100%. Some hypotheses include:
- Individuals have orders of magnitude differences in the amount of aerosols they produce, this could lead to some people just never becoming contagious
- The period of maximum contagiousness may be as short as 12 hours. If housemates / spounses happen to not interact with each other in this window, the chance of infection drops.
- Housemates / partners may isolated from each other upon noticing symptoms, which reduces the chance of transmission.
- The hourly rate of transmission is likely non-linear, i.e. 3 hours in a row with someone is likely less risky than 3x the risk of 1 hour.
The original household member estimate comes directly from Curmei et al. meta-analysis. The partner estimate is very speculative, based on adjusting Curmei et al. using a datapoint from Li et al.. We increased the household transmission rate for delta based on Allen et al.. We scaled the partner transmission rate based on the same study. See Research Sources for slightly more detail.
To learn about the scientific research supporting our estimates, please see the Research Sources section.
How likely is it that the other person has COVID?
Now we understand Activity Risk, or how your chance of getting the virus changes based on the activity you’re doing. But Activity Risk assumes the other person is COVID-positive. What are the actual chances that whoever you're interacting with has COVID? Let’s look at Person Risk to understand that.
The Calculator and Risk Tracker include a more detailed breakdown of different mask types with different multipliers. Our masks research section explains the detailed sources and reasoning for these different types. ↩︎
Person Risk
Person Risk is the chance that the other person currently has COVID. This is based on overall prevalence in your area and their recent behaviors.
So you’ve decided to meet a friend for lunch. You know the Activity Risk is 14% per hour (for an indoor unmasked lunch) and much less if you MODify your hangout. But the Activity Risk assumes that they currently have COVID.
What’s the chance that your friend actually has COVID? They aren’t coughing and they feel totally fine. Can you conclude they aren’t infected? Unfortunately, no. Roughly 55% of COVID transmissions happen when the person has no symptoms.[1]
- Not all diseases work this way. For example, Ebola is only contagious when the person is already exhibiting symptoms. However, COVID is a different disease, and one of its defining features is that it has a high rate of transmission from people who don’t yet have symptoms.
This means that the chance someone has COVID (which we’re calling “Person Risk”) depends on their actions and choices in the past 10 days or so, not just whether they’re actively showing symptoms.
We use three different methods of guessing someone’s chance of having COVID.
- The Basic Method is to just assume the person is “average” for their region. The chance your friend has COVID is the chance that anyone in your geographic area has COVID.
- The Advanced Method is to add up the risk of each individual activity that person has done recently.
You do not need to understand exactly how these methods work to use the calculator, but if you want to create your own custom estimates for specific people in your life then we strongly recommend learning to use the Advanced Method and the associated risk tracking tool.
Skip ahead and takeaways
If you would like to skip ahead, please first read the following takeaways that we think are the most important things conveyed in the next few sections:
- The chance someone has COVID is very different in different geographic regions.
- The very same activity that is fairly safe where I live might be fairly dangerous where my parents live, because the risk that people have COVID there is higher.
If you would like to understand how we use the basic and advanced methods to calculate Person Risk, read on.
Skip ahead to Putting it all together, or read on about the Basic Method for more detail.
Note that this figure includes both presymptomatic transmissions (where the person transmitting COVID will eventually show symptoms, usually within a few days, but hasn’t yet) and asymptomatic transmissions (where the person transmitting will never show symptoms). Catching COVID from someone presymptomatic is much more common: this accounts for about 50% of all transmissions, as opposed to asymptomatic transmissions which account for only about 5%. The COVID discourse tends to muddy this fact somewhat. Asymptomatic infections are inherently harder to measure (because you probably won’t get tested if you don’t show symptoms), and there are indeed plenty of them. However, most of them don’t infect anyone else. ↩︎
The Basic Method of calculating Person Risk is the regional average
As we know, prevalence varies widely across different geographic locations. For example, at the time of writing, Sydney has much lower rates of COVID than San Francisco. So the Person Risk from your friend in Sydney will be much lower than the risk from your friend in San Francisco.
The Basic Method is to just assume that a person is “average” for their region. The chance your friend has COVID is the chance that anyone in their geographic area has COVID.
How we estimate the regional average
To estimate the chance that a random resident in your area has COVID, you need to figure out the number of new infections last week in your area. This is because a typical person is infectious for about a one-week period.[1]
We will give an overview of the steps, then explain the steps in more detail.
- Start with the number of new reported cases in your region last week. The calculator does this automatically for you, or you can look up these numbers manually by Googling.
However, this is just a start. You cannot use this number directly because it underestimates how many people are actually sick. You need to take into account two important factors.
-
The first factor is underreporting. Many people with COVID won’t ever get counted in the official statistics. They might not think their symptoms are anything unusual, so they don’t get tested. Or they might not be able to access testing.[2]
-
The second factor is delay. There’s a delay of 1-2 weeks between when someone becomes infected and when their positive test result comes back. The true number of confirmed cases who were sick last week isn’t known yet, and won’t be known until those tests come back next week. If cases are rising, last week’s statistics will be too low.
The calculator can look up new reported cases automatically, and takes these adjustments into account as well.
The chance someone has COVID is very different in different geographic regions.
While we were working on this writeup, in July 2020, we calculated the Person Risk (Basic Method) in San Francisco as about 5107-in-a-million, and about 84-in-a-million in Sydney.
This means that the risk of doing a specific activity in San Francisco that month was about 60 times higher than doing the same activity in Sydney.
Inviting one random person over for coffee (indoors, unmasked, undistanced) in San Francisco would’ve been about as risky as inviting 60 random Sydney residents to your home!
There is not just one answer for “How risky is it to invite one person over for coffee?” It depends on where they live and how widespread COVID is there.
Detailed steps for Basic Method
To learn how do these steps manually, or to understand how the calculator does it, read the rest of this page.
Step one: Look up reported cases
To estimate the prevalence of COVID where you live, start by looking up the number of reported cases last week in your region.
- Make sure to look up new cases, not total cases.
- Make sure to get statistics for a week, not a day.
You decide how to define your region. This might be based on the county where you live, or you might want to include multiple counties if you live in a major metropolitan area. If data is limited, you might have to use your entire state.
If you live in the US, you can use the CovidEstim website. This gives daily new reported cases per 100,000 people. To get a week’s worth of cases, you’ll need to calculate: daily new reported cases per 100,000 people * 7 days.[3] You will then use 100,000 as the population.
Step two: Underreporting factor
Many people with COVID won’t ever get counted in the official statistics. The official statistics are underreporting the real number of new infections.
You can use the positive test rate (the percentage of tests that come back COVID-positive) as some evidence about how many infections are being caught by testing. Ideally, the positive test rate should be very low, indicating that contact tracing is working to find all contacts of an infected person, and that testing is available for each contact. If a high percentage of tests are coming back positive, then there are probably a lot more infected people out there than the testing data shows.
If you live in the US, you can look up the positive test rate in your state at CovidActNow.
We use the correction factor proposed by COVID-19 Projections:
prevalance_ratio = 1250 / (day_i + 25) * positive_test_rate ** 0.5 + 2
true_infections = prevalance_ratio * reported_infections
where day_i = number of days since 2020-02-12
More details are available in Research Sources or on COVID-19 Projection's website.
Step three: Delay factor
Since test results take about one week to come back on average, the number of new reported cases in your region last week really represents the number of new positive test results in your region the week before that. The results are delayed.
If cases are flat or falling, it’s fine to use this number as is.
If cases are rising, then we need to estimate the increase by comparing last week’s reported case numbers to the week before that. For example, if last week there were 120 reported cases, and the previous week there were 80 reported cases, then the weekly increase is 120 / 80 = 1.5. We would use 1.5x as our delay factor. To avoid over-extrapolating from a single superspreader event in an otherwise low-prevalance area, we have capped the delay factor at 2x
- In the calculator this would be displayed as a 50% increase in cases from last week to this week
Step four: Estimate number of new infections last week
Use this equation to combine the previous three steps to estimate the regional prevalence of COVID in your area:
New Infections Last Week = Reported Cases ⨉ Underreporting Factor ⨉ Delay Factor
Step five: Divide by population to get a final estimate
From there, calculate the basic Person Risk by comparing the new infections last week with the overall population in your region.
Person Risk (Basic) = New Infections Last Week / Population In Millions
Example Sydney and San Francisco calculations
Here are two examples:
Sydney in July 2020 (lower prevalence)
-
Step 1: As of July 26, 2020, the state of New South Wales in Australia (where Sydney is located) had 81 reported cases in the last week, and a population of around 7.5 million.
-
Step 2: The week before that, there were 62 reported cases.
81 / 62 = 1.3so we’ll use a 1.3x delay factor, i.e., a 30% increase in cases from last week to this week. -
Step 3: The percentage of positive COVID tests is extremely low:
81 cases / 135,089 tests = 0.05%so we’ll use our minimum 6x underreporting factor.[4] -
Step 4: Therefore,
81 reported cases * 1.3 * 6 = 632 new infections last week. -
Step 5: So the Person Risk (the chance that a random resident in New South Wales has COVID) is
632 infections / 7,500,000 people = 0.000084 or 0.0084%.- An easier way to talk about this tiny number is to multiply it by a million:
0.000084 * 1,000,000 = 84. - This is the same as if we had just divided by
7.5(the population in millions).
- An easier way to talk about this tiny number is to multiply it by a million:
So if all you knew about a person is that they lived in New South Wales in July 2020, their Person Risk at the time would’ve been 84, which means there’s a 84-in-a-million chance that they had COVID (in that particular week).
San Francisco in July 2020 (higher prevalence)
Compare this with San Francisco County in California, which had 749 new reported cases during that same week, and a population of 0.88 million.[5] Cases at that time were declining, so we won’t use a delay factor. The positive test rate was 4.3%, so we’ll use a 6x underreporting factor. Therefore, 749 reported cases * 6 = 4494 new infections last week. To get the Person Risk, divide by the population (in millions): 4494 infections / 0.88 million people = 5107.[6] So a resident of San Francisco had a Person Risk of 5107, or a 5107-in-a-million chance of currently having COVID (for this particular week).
Comparing the above examples
5107-in-a-million (in San Francisco) is about 60 times higher than 84-in-a-million (in Sydney). So the average Person Risk in San Francisco is 60x as high as in Sydney!
The most-infectious period starts a couple days after infection, but the day-to-day noise in new case numbers is enough that “0-7 days ago” and “2-9 days ago” are unlikely to be meaningfully different. See Research Sources for more about the infectious period. ↩︎
As an example, New York City in March–April 2020 was completely overwhelmed by COVID, with widespread reports that even people with obvious and severe symptoms were unable to receive a test. We’ll look specifically at the five boroughs plus Westchester, Nassau, and Suffolk counties, an area containing 12.2 million residents. A survey for COVID antibodies in these counties performed between April 25–May 6 found that 23% of people had previously been infected, but according to the Johns Hopkins dashboard only 263,900 cases (2.2% of the area’s population) had been officially recorded by May 1. ↩︎
It's not very obvious from their website, but CovidActNow's daily numbers are smoothed by taking the average over the past 7 days. Thus, this calculation will correctly compute the number of cases last week, not just 7 times the number of cases yesterday. You might find that other sources of data do this as well. ↩︎
With this low of a positive test rate, an even lower underreporting factor is quite plausible, but we don’t have enough data to estimate just how low we should go. ↩︎
Tip: if your data source lists a “7-day moving average” of cases on a certain day, the number of cases in the preceding week is just 7 times that. ↩︎
This seems high to us: a 5107-in-a-million chance over a week-long period of getting COVID from being an average SF resident implies the average SF resident has a 23% annualized chance of getting COVID. That seems pretty bad. We really hope we’re wrong somewhere and the real number is lower; perhaps we don’t need as high as a 6x underreporting factor anymore? ↩︎
The Advanced Method makes a list of the person’s recent behavior
To get a more accurate estimate for Person Risk, we can actually add up the risk (in microCOVIDs) of their recent behavior. Remember, a single microCOVID represents a one-in-a-million chance of getting COVID.
The Advanced Method is to add up the risk of each individual activity that person has done recently.
The Risk Tracker is a tool that can help you add up activities in the Advanced Method.
Just like you can calculate this for each of your actions, you can also calculate it for your friend’s actions, using the same formula:
Cost = Activity Risk ⨉ Person Risk
We can do this by looking at all of their activities between 2–9 days ago[1] and determining the risk of each individual activity. Or if they do the same things every week, what does their typical week look like?
This is an advanced method because it requires asking about and calculating the risk of each of your friend’s recent or typical errands, hangouts, and other activities. And you might have to ask about your friend’s contacts too!
Add up the person’s socializing, errands, and work
The advanced method hinges on getting an accurate picture of all of your contacts' activities and risks. This requires examining their lives in more scrutiny than you may be used to in normal times. To help, we've developed a list of questions to ensure you are thorough in assessing their risk.
We think about risk in three categories: socializing, errands, and work. To calculate total Person Risk using the advanced method, you can add these three categories together, as follows:
Person Risk (Advanced) = Socializing + Errands + Work
Note that this formula uses addition, whereas everything else we’ve done until now has been multiplication.
For socializing, just estimate each social activity in microCOVIDs (using “Cost = Activity Risk ⨉ Person Risk”) and add them together. This is the place to count the exposure from all their household members as well.
Errands include grocery shopping, transit, and other public settings. These can be harder to estimate individually; we have some guidelines in the Q&A.
Work is modeled just like the above socializing and errands, and you would ask similar kinds of questions: how many people is this person sharing indoor air space with? For how many hours per week? What is their risk profile like?
Though you can do Advanced Method calculations on your own, the Risk Tracker was designed for that very purpose. It is a helpful tool for both individuals and households/pods who want to manage their risk.
The best way to understand how to apply the Advanced Method is through an example. See the next section for a detailed example.
The 2-9 day window is an approximation for people who keep relatively constant schedules or maintain a similar level of risky behaviors week over week (for instance, by using microCOVID to track their own activites). If this is not a good description of the person's behavior (e.g. they recently took a flight, went to a party or indoor restaurant, or had contact with someone with COVID), it is necessary to count up all their activities from the last 2-23 days (3 weeks). Events past 5 days have diminishing effects on their riskiness, which makes this method difficult to do by hand. The Risk Tracker handles this calculation for us. For details on how this is derived, see Research Sources. ↩︎
Comparing Person Risk methods with an example
Let’s work through a quick example to compare the different approaches for estimating Person Risk.
Reasonable Rosie lives with one roommate in San Francisco and works from home. Rosie grocery shops twice a week in a surgical mask. Nobody else visits Rosie’s apartment, and she doesn’t hang out with anyone else indoors. She went on 5 separate 1.5 hour masked, outdoor, regular distance (3-feet (1 meter) apart) walks with friends over the past ten days. For simplicity, we’ll assume her roommate does the exact same set of activities that she does.
You’re planning to hang out with Rosie and want to know her Person Risk, so you can know what precautions to take. You calculate:
- Basic method: 5106 Person Risk.
- Because we estimate the San Francisco prevalence of COVID infection (at the time of writing) as 5106-in-a-million. This would change if prevalence changed.
- Advanced method: 217 Person Risk
-
Remember, here you’re calculating Rosie’s own risk of getting COVID from her activities, in microCOVIDs, which you can then use in calculating your risk of getting COVID from her.
-
Each walk starts with a 14% Activity Risk (for one-time contact per hour) times 1.5 hours, and then gets a decrease of 2x for Rosie’s mask, 4x for her friend’s mask, and 20x for being outdoors. Since she stays 3 feet (1 meter) apart from friends on these walks, there is no additional reduction for distance. We’ll treat the friends as average residents (using the 5106 Person Risk from the Basic Method above). Five walks in the past ten days adds up to
0.14/hr ⨉ 1.5hr ⨉ 5 ⨉ 5106 ⨉ (1/2) ⨉ (1/4) ⨉ (1/20) = 34microCOVIDs. -
Rosie also goes to the grocery store twice a week. We estimate this as spending 2 hours per week, about six feet (two meters) away (2x) from 5 random people at a time (each with 5106 Person Risk using the Basic Method), wearing a surgical mask (2x). Let's assume the other people in the store are wearing thick and snug cloth masks (3x, not as protective as surgical masks), but that people are not talking (5x decrease). Rosie’s grocery shopping adds up to
5106 ⨉ 0.14/hr ⨉ 2hr ⨉ 5 ⨉ (1/2) ⨉ (1/3) ⨉ (1/5) = 238microCOVIDs. -
So Rosie’s errands plus her walks gives her a risk of
238 + 34 = 272microCOVIDs (or 272-in-a-million chance of catching COVID). -
If Rosie’s roommate does the same things (two hours of grocery shopping and five walks with friends per week), then Rosie’s roommate’s risk of getting COVID, in microCOVIDs, due to sources other than Rosie, is the same: 272. Multiply this by the 40% Activity Risk of being a roommate and you learn that Rosie’s roommate poses a risk to Rosie of
0.40 ⨉ 272 = 109microCOVIDs.[1] -
So the total COVID risk for Rosie, based on her behaviors, is
238 + 34 + 109 = 381microCOVIDs. Now you can use this number as the “Person Risk” when you’re calculating your own chance of getting COVID from Rosie.
-
One thing you will notice is that when we re-compute Rosie's Person Risk via the advanced method, we get substantially smaller numbers. This is because the Basic method assumes Rosie is about average, which is not true. In fact, she is being about ten times more cautious than the average person in her geographic area. The more you know about a person’s behavior, the more accurate your estimate can be. In some cases it might go up, in other cases it might go down.
With a total COVID risk of 381 microCOVIDs, Rosie is being much more cautious than average![2] It’s also possible we’re still overestimating her risk, even using the Advanced Method. For example, if her friends are similar to her, then they are probably more cautious than average as well, which would reduce her COVID risk from socializing.
In our calculator we’ve provided some Person Risk Profiles that were made using the Advanced Method. You can use them as a starting point to create your own calculations.
Now that we’ve looked at Person Risk, we can combine it with Activity Risk to get the cost in microCOVIDs of a given activity. Hooray, you made it!
If the people in your household/pod have any significant exposure to the outside world (including groceries, essential work, etc.) then you will need to include your own contact with your housemates (or others in your pod) in your estimate of how many microCOVIDs of exposure you have incurred, because those people’s Activity Risk is not zero. The fact that they are in your pod does not change the fact that everything they have done in the past 10 days poses a risk to you. See our household/pod documentation for more info on managing risk in that setting. ↩︎
If Reasonable Rosie keeps up this rate of 381 microCOVIDs per week, she’ll incur about 20,000 microCOVIDs per year, which implies about a 2% chance of getting COVID during that year. This is much lower than the average American! ↩︎
Putting it all together
We can now multiply Activity Risk by Person Risk to get the microCOVID cost of a given interaction.
Cost = Activity Risk ⨉ Person Risk
Multiple-person interactions
So far we have assumed you are interacting with just one other person (a picnic with one friend, just one other person in the restaurant, etc).
If you are interacting with multiple people (lunch with two friends; being near five people at a time in a grocery store), you can add the microCOVID costs together, i.e., multiply by the number of people.
Cost = Activity Risk ⨉ Person Risk for one person ⨉ Number of people
In the calculator we display the Person Risk for each person.
An example of combining Activity Risk and Person Risk to get a total Cost
Let’s say you would like to spend an afternoon catching up with Reasonable Rosie (from an earlier example), whose Person Risk is 381 using the Advanced Method. An indoors meetup has a 14% Activity Risk per hour, so it costs you 14% per hour ⨉ 2 hours ⨉ 381 Person Risk = 107 microCOVIDs.
107 microCOVIDs = 14% per hour (Activity Risk) ⨉ 2 hr ⨉ 381 (Person Risk)
If you both wear surgical masks, it costs you 8x less: only 13 microCOVIDs. And if you hang out outside instead of inside, it costs you an additional 20x less, for just 0.7 microCOVIDs (less than 1 microCOVID!)
0.7 microCOVIDs = 14% per hour ⨉ 2 hr ⨉ (1/8 masks) ⨉ (1/20 outdoors) ⨉ 381 (Person Risk)
Should you do these activities? It depends on how important you believe it is to avoid COVID (for your own health, and to protect others), and how important seeing Rosie is to you!
- If you’re aiming for 1% risk of COVID per year (833 microCOVIDs per month), an indoor unmasked hangout with Reasonable Rosie is something you can do multiple times per month, and you can treat the outdoor masked hangout as totally “free.”
- However, if you’re aiming for 0.1% risk per year (83 microCOVIDs per month), one unmasked indoor hangout with Reasonable Rosie is more risk than you'd be willing to spend in an entire month. To spend your microCOVIDs more efficiently, you’ll want to use protective measures like wearing a mask or only hanging out outdoors. Unless, of course, Reasonable Rosie is the only person you want to see all month and you don't need to do groceries.
- And if you’re highly vulnerable and aiming for 0.01% risk per year (8.3 microCOVIDs per month), the outdoor mask walk is something you can afford to do, but you cannot hang out indoors with Reasonable Rosie even once without jeopardizing a large fraction of your budget for the entire year.
Now that you have seen the whole process end-to-end and several example numbers, it might be a good time to revisit “How much is a microCOVID?”.
Remember that Reasonable Rosie is a specific example person, from a specific example place and time. Her risk of having COVID depends on her recent hypothetical behaviors. If you’re hanging out with someone at a different place or time, the Activity Risk would be the same, but the Person Risk is likely to be very different, and so the overall Cost would be very different.
Calculator and Conclusion
Calculator
While it's good to know how the math works, it can be a bit drudgerous to actually sit down and do it for every activity you're considering. With that in mind, we developed a calculator tool to help you estimate and multiply the Person Risk and Activity Risk, including any modifiers for safer behavior (like wearing a mask), to get an estimated number of microCOVIDs from a given activity. Just give it your location and tell it about the activity you'll be doing, and it will tell you the “cost” of that activity in microCOVIDs.
We think it’s especially powerful as a way to hone your intuition. Try putting some of your activities from last week into the calculator. Which activity had the largest cost? How many microCOVIDs do your actions add up to?
Conclusion
We hope our mindset towards COVID risk modeling helps you feel less trapped and more free to live a safe(r) COVID life.
If you have more questions, check out the supplementary Q&A section coming up next, and/or the Research Sources section after that.
If your questions aren't answered in the supplementary material, or if you'd like to offer feedback or are interested in contributing to the project, please contact us. We would love to hear from you!
Thanks for reading!
If you've found this paper or the calculator valuable, consider supporting the project with a small donation. We are all unpaid volunteers and we don't currently have any funding to work on this project. Thank you in advance!
Q&A
Jump to: General | Activity Risk | Person Risk | Vaccines | Specific Activities | Related Work
General Q&A
How should I choose my annual risk budget?
We currently have two main risk budget options. You are, of course, welcome to choose any risk budget for yourself.
| Title | Risk of getting COVID per year | Weekly microCOVID budget | Suggested for.. |
|---|---|---|---|
| Standard Caution Budget | 1% chance of getting COVID per year = 10,000 microCOVIDs per year |
= 192 microCOVIDs per week | Healthy people NOT in close contact with more vulnerable people |
| High Caution Budget | 0.1% chance of getting COVID per year = 1,000 microCOVIDs per year |
= 19 microCOVIDs per week | Suggested if you or your close contacts are more vulnerable to COVID. |
Vulnerability increases with age. We think age over 60 confers substantial increased vulnerability to severe illness from COVID. Certain underlying medical conditions also confer increased vulnerability:
- BMI of 30 or higher
- Type 2 diabetes mellitus
- Smoking
- COPD or other heart conditions
- Cancer
- Chronic kidney disease
- Immunocompromised from solid organ transplant
- Sickle cell disease
Risk to you & risk to others
When choosing your budget, you want to factor in two important aspects: risk to you, and risk to others.
-
Risk to you: If you are in the under-40 age bracket and do not have other risk factors, then a 1% chance of COVID per year puts your risk of disability due to COVID at about the same level as your risk of disability due to driving a car. See below for how we arrived at the 1% annual risk budget.
-
Risk to others: Even if you are personally comfortable with risk-taking, it’s important to choose a lower risk tolerance in order to protect vulnerable members of your community. Here are a few ways to think about that:
-
If you get COVID, on average you will pass it to at least one other person, who in turn will pass it to others. Eventually it will reach someone who is at very high risk of death. By avoiding getting infected yourself, you are protecting these vulnerable members of your community.
-
A useful ethical rule-of-thumb is to behave in a way that would be good if everyone behaved that way. So, we can ask: what risk tolerance would keep the pandemic at manageable levels if everyone followed it? In most places in the US right now, a 1% yearly risk of COVID would keep the pandemic at manageable levels. For public health reasons, we wouldn’t recommend voluntarily choosing a risk tolerance higher than 3%.
-
Some people (such as essential workers) have no choice but to run a high risk of getting COVID. Containing the pandemic across society only works if those of us who do have a choice choose to take fewer risks.
-
How did you arrive at a 1% annual risk budget?
We think roughly 1 in 10 COVID cases lead to long-term negative health consequences for the infected person ("long COVID"). Data from the UK's Office for National Statistics suggests that 13.7% of COVID-infected people may continue to experience symptoms after 12 weeks and 12% continue to experience symptoms after 18.5 weeks.[1] That would mean that a 1% chance of COVID is the same as up to a 0.12% chance of ongoing negative health consequences from COVID for at least 4 months.
The average American drives 13,476 miles per year. In 2018 there were 2,491,000 car-crash-related injuries (of any severity) spread across 3,240,327,000,000 vehicle miles travelled (see the NHTSA website for more detailed breakdowns). A study of Swedish car crash injuries found that 11.4% of them met the criteria for at least “1% permanent medical impairment” five years later. (“Permanent medical impairment” is a legally-relevant concept that attempts to quantify disability, and the 1% level was the lowest level of disability that was discussed in the Swedish car crash study.) Multiplying this out, we get a 0.11% chance of ongoing negative health consequences from driving for one year.
You may choose to follow a different risk budget. Here is some information that might be helpful in deciding what is right for you:
- Among people under 40, the chance of death from COVID is about 0.1-0.2% (Our World in Data)
- Among people over 60, this rises to 2-3% and doubles with every 10 years over 70.
- A 0.1% chance of death is equivalent to...
- Driving 100,000 miles (IIHS)
- Base jumping 3 times (Wikipedia)
- 167 skydiving jumps (Skydive California)
Also remember that, if you take on personal risk, you also present a risk to others. Take care to isolate from others who do not consent to your risk tolerance.
If there’s a precaution I don’t see a multiplier for here, should I still do it?
Yes, definitely! The most important such precaution, in our opinion, is communication around symptoms:
- Ask people directly and clearly if they have any symptoms, right before hanging out with them. Even if they only have “mild” symptoms that seem like “nothing to worry about,” consider if you can take a rain check, or at least MODify your hangout.
- If you have any more concerning symptoms[2] then immediately notify anyone you saw in the past 10 days, and contact your doctor for medical advice.
- If a household member develops more concerning symptoms, follow CDC best practices for home isolation straight away while you contact a doctor for medical advice.
Other important precautions include washing & sanitizing your hands, covering your sneezes with your elbow including when you are at home, using a better-fitting mask, and wearing eye protection (we particularly recommend wearing goggles and a P100 mask if you are looking for extra safety when shopping!)
Activity Risk Q&A
What if I hang out with someone indoors for a long time? If we hang out for 3 hours, that’s an Activity Risk of 14% ⨉ 3 = 42%, which is slightly more than the risk for a household member.
In the case of a long indoor hangout, we suggest just to cap the total Activity Risk at the household member number (40%). Or if you’re cuddling or being intimate, cap the total Activity Risk at 60% as mentioned above for spouse/partner. These are not particularly principled answers. As we’ve mentioned in footnotes before, the ability to just add microCOVIDs (rather than multiplying probabilities) starts to break down as probabilities get larger. Additionally, the data we’re basing our guesses off is more relevant to the smaller risks that we more commonly see with typical activities. Certainly don’t use an Activity Risk larger than 100% for anything.
If you live with multiple people, do you account for the additional risk of a longer infection chain within the household?
No. We’ll explain what this means and why we don’t account for it in the specific case of a single household.
Imagine I live with Alice and Bob. Alice gets sick. There are two things that could happen next that could get me sick:
- I get it directly from Alice.
- I don’t get it from Alice, but Bob does. Then Bob infects me!
There’s a 40% chance that I get sick directly from Alice. There’s a 60% * 40% * 40% = 10% chance that the second scenario happens instead. So you might think the total risk to me should be more like 50% than 40%.
We currently don’t model this effect, and we think that’s pretty safe if (and only if) you and your household members are conscientious about monitoring for symptoms and isolating from one another at the first sign that someone in the house is feeling unwell. Such isolation should include some reduction in contact between the household members that still feel fine, since one or more of them might have become infected by the unwell person before their symptoms appeared.[3]
Here’s why isolating helps reduce this source of error:
- Prompt isolation means it’s less likely[4] I get it directly from Alice, and less likely that Bob gets it and can pass it to me.
- Even if Bob ends up getting sick, Bob and I can start avoiding each other immediately, as soon as Alice gets symptoms. Although it’s quite possible for Alice to give COVID to Bob before Alice has symptoms, it’s much less likely for Bob to pass it on to me before Alice has symptoms.[5]
As a result of these considerations, we don’t think we’re making a huge error by using the unadjusted 40% number for the Activity Risk of having a house hold member.
Of note here: while full isolation is the gold standard for reducing infection risk, it’s useful to also have some lighter-weight tools that you can deploy if you’re uneasy about infection risk for some reason but not uneasy enough to find hard isolation to be worth the (admittedly considerable) social and practical costs. Extrapolating from the MOD factors, we think wearing a mask around the house for several days probably reduces your risk of infecting your housemates by about 4x, which is a lot of protection to get from a relatively simple intervention. In the authors’ household we deploy this one if we’re feeling at all unusual, even if the symptoms (such as a scratchy throat) aren’t suggestive of COVID; or if we’ve recently done something moderately higher-risk than usual.
Why do I need to account for my household members? I thought it was “free” to hang out with people as often as I want, so long as they’re all in the same “bubble”?
So long as the people in your “bubble” have some risk of getting infected from anywhere, the risk they pose to you contributes to your total microCOVIDs.
In short, we think “closed quarantine bubbles” are a good strategy for very-low-risk groups who don’t venture outside the house often, but make less sense for larger bubbles with more exposure to the outside world.
To spell it out a bit more: If nobody in your bubble has any exposure to other people or public spaces outside the bubble, then in fact you can count their Person Risk as very minimal.[6] This isn’t a magical property of the bubble being "closed" per se; it’s a result of everyone only socializing with other people who also have very minimal Person Risk. Seeing a friend who lives completely alone and literally never leaves the house would also keep you at this same low risk level. The “closed bubble” framework is a way to coordinate around maintaining a very low risk level together.
But if people in the bubble are doing things that expose them to others somewhat—going to work, grocery shopping, taking trips—then even if they aren’t meeting up for coffee, dates, or events with anyone outside the bubble, they still have some nonzero Person Risk, and you should multiply this with the Activity Risk of seeing them.
This means that, if the people “in your bubble” have some exposure to the outside world, then reducing your total amount of contact is likely more important than making sure you are only seeing people in your bubble.
To summarize, reducing your total amount of contact (and choosing to socialize only with other people who are also reducing their total amount of contact) is (we think, for most people) the most important strategy for staying safe.
So if my housemate really wants to see a partner in another house, you believe it is sometimes better from a risk standpoint not to negotiate for the partner’s entire house to get added to a closed bubble with us?
Right! To illustrate, compare the following two scenarios:
-
The two houses merge into one large “bubble”. Everyone gets together for a full group dinner between the two houses.
- This could be quite a large gathering, where everyone is exposed to everyone. If any of these people have been to work, on public transit, or in stores, then everyone at the dinner is indirectly exposed to those external sources of risk.
-
No specific bubble arrangement, but nobody else in your house socializes with anyone else in the other house. Just your housemate sees just their partner, in the partner’s room with the door closed.
- One person is exposed to one other person. This is less overall contact.
- Of course, if you choose not to make a “closed bubble” agreement, the partner might be doing other socializing of their own.
Which strategy is less risky depends on which factor dominates: the partner’s other socializing, or every bubble member’s combined external exposure. This is why we think closed bubbles are the safer choice for people who are generally not working outside home or going out at all, and reducing total contact is the safer choice for people who have a moderate amount of external exposure. We haven’t done the math on this yet, and we would be interested to see an analysis of this.
MOD: Masked, Outdoors, and Distance
I was told to wear masks to protect others, not myself. Do masks actually protect me?
Yes! Cloth masks and surgical masks protect others more than they protect you (see Research Sources), but they still reduce your risk of catching COVID by half, so they’re well worth it even from a selfish perspective.
What about masks that provide more protection, like an N95 or P100 respirator?
These masks provide more protection than a cloth or surgical mask:
-
Masks that claim to have N95-like filter media (e.x. KN95, Vogmask), can be considered equivalent to KN95's - designed to filter, but not rigorously quality controlled or tightly fitted. These receive a 6x protection factor.
-
For a well-fitted, well-sealed N95, we roughly estimate an 8x reduction in risk for the wearer (versus 2x for a surgical mask or high-quality cloth mask).
- But remember, these masks are only effective if you get a tight seal around your face! Just “wearing an N95” doesn’t protect you all the way. We have seen a friend of ours “wear an N95” that was much too big for their face, leaving a big gap under their chin. Other friends have worn an N95 over a beard, but facial hair definitely prevents a good seal. One study shows that even a pair of tiny points of leakage a couple of millimeters in diameter dramatically increases the number of aerosol particles that can pass through a high quality mask. Please do a seal check and watch a video in order to effectively use your N95.
-
A P100 is even better. We estimate that P100's provide a 20x reduction in risk.
- A major reason we like P100s is they are easier to get a good seal on. You can search for online training on how to do this.
- Note that P100 respirators typically have an outflow valve, meaning they provide minimal protection to others from you, so if you use a P100, you may be legally required to cover the outflow valve with cloth or a surgical mask.
What P100 do you recommend?
We absolutely love the GVS Elipse. They're available on eBay for $60-90.
Is it reasonable to just multiply together all the modifiers? 8x for masks, 10x for outdoors, and 2x for 6ft of distance?
Each of these modifiers changes the total number of particles that might reach you, so we do think it’s reasonable to keep piling them on somehow. How exactly they combine is not precisely clear. But if you consult the Research Sources section, the masks and distance modifiers were estimated from data including healthcare settings where they were sometimes combined.
The “outdoors” modifier is the one we have the least confidence of. At larger distances, we speculate that outdoors might provide more than 20x protection, because particles have more time to diffuse upwards into the vast empty space above everyone’s heads, whereas indoors small particles could hang in the enclosed room air. On the other hand, at smaller distances (especially at close range: cuddling, tango dancing, etc.) we don’t have any reported data that we feel sheds light on how much of a protection factor there might be, so we suggest not to use the 20x modifier for outdoor interactions with unusually close range or with other factors associated with superspreader events (yelling, dense crowds, etc.).
Person Risk Q&A
Are people who work outside the home riskier than people who work from home?
We do not think that, as a blanket rule, every person who works outside the home is riskier than every person who works from home. Activites outside of work play a major role in a person's chances of contracting COVID.
For instance, a Healthcare Worker who wears a sealed N95 mask while seeing one unmasked patient at a time for 40 hours per week, but does not see any other people in a typical week, would be calculated as follows:
average_risk * 40 hours * 14%/hr * 1/8 (N95) = 0.7 * average_risk
Therefore, this worker could be less risky than the average person in the area (although the final risk will depend on what else they are doing in terms of chores and socializing).
We recommend using the Advanced Method to estimate the risk of all your close contacts, rather than using blanket risk categories. The Risk Tracker is an excellent tool for keeping a tally of one's personal risk. The microCOVID team includes a Primary Care Provider who tracks and reports her risk using this tool, which suggests that her weekly risk is on the order of 100microCOVIDs per week.
We originally proposed an "Intermediate Method", in which people who work outside the home are guestimated at 2x or 3x the population average. This was based on the following two studies:
- Chamie et al. found a 6x higher positive test rate among frontline service workers.
- Data from Washington State suggested Heath and Social Service workers had been infected at 2x the average rate.
However, we have retracted this method for the following reasons:
- These studies include data early in the pandemic when COVID-19 was poorly understood and good PPE was unavailable.
- It appears that the average person has become significantly riskier since early in the pandemic (more social activity / less lockdown yields high overall rates).
- These categories of people are highly heterogenious. Lumping them all together makes no sense.
- Differences in PPE alone can reduce transmission risk by 10x, which would be a larger effect than either of these studies.
- Many hospitals have precautions that decrease the liklihood that a random healthcare worker will be exposed to COVID.
- On the other hand, some healthcare workers directly work with confirmed COVID patients, which is a much higher risk category.
- Various studies, such as Baker et al. have shown that, for at least some pockets of healthcare workers, healthcare workers are no more likely to get infected through their work than the average person is to get infected through socializing.
- The above Washington State report shows that people who work outside the home got COVID at about the average rate for the state.
Vaccines Q&A
How should we think about people who have been vaccinated?
*Summary: Vaccinated people receive a multiplier on all incoming microCOVIDs from their activities. The multiplier depends on which vaccine they've gotten and is contingent on having waited long enough for their immune system to respond.
People who have been vaccinated are less likely to catch COVID and transmit it to others, which results in them getting fewer microCOVIDs from activities. However, they are not totally immune to COVID, and it is quite easy for a vaccinated person to counteract the decreased risk per activity by doing lots of risky activities (for instance, the Moderna vaccine confers a 1/10x multiplier for incoming microCOVIDs, so a vaccinated person who does 10x more risky behavior after being vaccinated would be just as many microCOVIDs as before).
There are two questions that are important for understanding vaccines:
- How much less likely is it for a vaccinated individual to catch COVID? This determines the reduction in microCOVIDs a vaccinated individual receives from a given action.
- If a vaccinated individual contracts COVID, how much less (or more) likely is this to result in negative consequences (hospitalization or death). This determines how much a person can increase their microCOVID budget for being vaccinated (on top of being able to do more activities from part 1).
1. How much less likely is it for vaccinated individuals to catch COVID? (Reduction in microCOVIDs)
Below is our best estimates for the vaccine efficacies for various vaccines. These are based on a weighted average of the efficacy of each vaccine vs. symptomatic and never-symptomatic COVID-19 infections. See Research Sources for the full derivations.
| microCOVID multiplier 14 days after 1st dose | microCOVID multiplier 14 days after 2nd dose | microCOVID multiplier 14 days after 3rd dose | |
|---|---|---|---|
| AstraZeneca | 1 | 1 | 0.3 |
| Moderna | 1 | 0.8 | 0.25 |
| Pfizer | 1 | 0.8 | 0.25 |
| Johnson & Johnson | 1 | 1 | 0.95 |
For perspective, the first dose of either vaccine confers equivalent protection as wearing a good quality cloth mask all day, every day on top of your actual mask and even when you normally couldn't wear a mask. Completing the 2nd dose of AstraZeneca’s or a single dose of Johnson & Johnson's vaccine confers more protection than wearing a surgical mask 24/7, and Pfizer or Moderna’s vaccine is as protective as wearing a KN95 mask all the time.
While the vaccines are nowhere near making you invulnerable to COVID, remember that these vaccines are absolutely game-changing — universal vaccination would reduce everyone’s chance of catching COVID by 50% or more. This will (likely) reduce the rate of community spread to the point that every week has fewer cases than the last (R<1). The end of the pandemic is in sight.
2. If a vaccinated individual contracts COVID, how much less (or more) likely is this to result in negative consequences? (Increased budget)
The Israeli government released data that suggests that citizens with Pfizer's mRNA vaccine were getting infected at 36% the rate of unvaccinated citizens, but hospitalized at only 7% the rate. This suggests the vaccine confers a 5x reduction in serious cases of COVID in addition to the reduces chances of getting COVID at all.
We have not done a thorough analysis of this effect in other vaccines.
We have not seen data that describes the effect of vaccines on long COVID in mild/asymptomatic cases. The 1% annual risk budget is based on risks of long term effects of COVID (as opposed to hospitalization or death). Reports of prevalence in long COVID in unvaccinated people varies widely:
- A study by ZOE found that "one in twenty people (5%) had COVID-19 symptoms for more than eight weeks, and around 2% of people can experience symptoms for 12 weeks or more". The data for this was self-reported and the researchers noted that many participants stopped reporting data before the conclusion of the study.
- Data from the UK's Office for National Statistics showed that, of a sample of 20,000 people infected with COVID, 13.7% continued to experience symptoms after twelve weeks.
- Another study early in the pandemic found lung abnormalities in half of asymptomatic COVID-19 cases on the Diamond Princess cruise ship. These lung abnormalities are similar to pneumonia; it is unclear from that study what percent led to long term health changes.
- Researchers found heart abnormalities in 78 of 100 recovered patients, sampling an average of 71 days after initial diagnosis. There may be self-selection bias among participants in this cohort.
As a result, getting a vaccination yourself confers a reduction in incoming microCOVIDs based on how the vaccine affects your chances of infecting others (as outlined above). You may additionally increase your budget based on how the vaccine reduces your own chances of negative outcomes, but this is a personal choice dependent on your own view of how averse to the various possible negative outcomes you are.
Some ways you may want to change your budget in after you and your close contacts are vaccinated:
- If you want to keep the same overall budget but live with housemates, you can increase your personal budget while maintaining the same annual risk; each housemate's activites has a reduced impact on others' microCOVID budget. I.e. if living with N housemates, before vaccination each person's allocation of microCOVIDs would have been
(200 / (1 + 0.4*N)). After everyone is vaccinated with three doses, this increases to(200 / (1 + 0.4*0.25*N)). - You may have been choosing your microCOVID budget primarily based on mitigating risk to others, rather than concern for your own health; When both you and the people you are trying to protect are vaccinated, you may increase your budget by 1 / vaccine multiplier (i.e. ~6x for the mRNA vaccines) while still having the same impact on them.
- If you are only concerned about the risk of your own hospitalization/death and unconcerned about effects of mild COVID or potential long-term symptoms, you may 5x your budget post vaccination.
Example A:
You live in a pod of 6. Prior to vaccination, all 6 housemates had a personal budget of 200 / (1 + .4 * 5) = 67 microCOVID/week. All 6 of you are now vaccinated with three doses.
- If all 6 of you agree you want to keep to a 200 microCOVID budget, you adjust the formula to
200 / (1 + .4 * .25 * 5) = 133 microCOVID/week. - If you agree to keeping the same impact on each other while individually choosing your own risks, you each may go up to
67 / 0.25 = 268 microCOVID/week. - If you all decide that you want to keep the same risk of getting severe COVID as pre-vaccination, you further 5x your budget (accepting a higher risk of mild/asymptomatic COVID).
Example B:
You live with or care for someone with a condition that reduces the efficacy of a vaccine (consult their doctor).
- You choose not to change your budget, since this person is just as likely to get COVID from you as before.
So is a vaccinated person safer to be around than an unvaccinated person?
Not necessarily. A person's risk is the product of their precautions and activities. It is true that a vaccinated person who does the same activities as a unvaccinated person will be less risky to be around. However, if the vaccinated person starts doing more risky behaviors, they could end up being more risky than before they got vaccinated! The only way to accurately understand a person's risk is to model each of their activities and multiply that total by the modifier from the table above. The Risk Tracker makes it easier to do this.
I heard that Pfizer’s vaccine is only 64% effective in Israel. Why is microCOVID treating it as 84% effective?
We dug into claims that the effectiveness of vaccines in Israel is 64% but had concerns about the methodology. These reports control for “age group..., sex, and calendar week” (Haas et al) but not individual behavior. Since Israel’s policy allows vaccinated individuals to participate in many activities with high risk of exposure (restaurants, movie theaters, etc. without masks), we hypothesize that the 64% effective number captures a combination of reduced efficacy of the vaccine vs the Delta variant AND increased opportunity for exposures.
Therefore, we used data from research in the UK that compared # of cases of the Delta variant vs the Alpha variant among vaccinated and unvaccinated individuals, which attempts to assess the vaccines’ efficacy in isolation (Bernal et al.), (Stowe et al.). These studies found 88% vaccine efficacy vs symptomatic COVID, which we adjusted to 84% to account for asymptomatic cases.
Specific Activities Q&A
Can I let a friend use the bathroom in my house?
We believe that if the person is indoors for <5 mins and wears a mask the whole time, then the risk will be negligible for all but the most cautious risk budgets. This is especially true if you can open a window to ventilate the bathroom space. See this article for more tips about this.
Silence? Singing, chanting, yelling? Speaking loudly? Exercising?
Based on the Jimenez Aerosol Transmission Model, we could contemplate up to a 5x reduction in risk for silence, and a 5x penalty for singing, chanting, yelling, or speaking loudly; plus an additional 5x penalty for heavy exercise.
Are small rooms riskier than large spaces?
Yes! Based on the Jimenez Aerosol Transmission Model and estimates of the total area of rooms of different sizes, we think you might consider the following multipliers: ×4 higher risk for a ‘tiny room’ (~10ft across) ×2 for a ‘small room’ (~15ft across) ×1 for a ‘normal room’ (~20ft across) ×0.5 for a ‘large room’ (~30ft across)
These assume you are already sufficiently distanced (at least 6 feet/2 meters) that the size of the room is relevant to the amount of aerosol you’ll breathe. In close quarters, we think the size of the room has less of an impact.
Should I use an extra multiplier for cuddling? Going on a date?
We personally use an additional multiplier of at least 2x for cuddling, Our original take on this was based on the assumption that our data for infection risk under “no particular distance” (which were largely collected in hospitals) reflect a distance closer to 3 feet (1 meter) than 0 feet. If each additional 3 feet (1 meter) adds a 2x improvement in safety, then being right on top of each other (0ft apart) might involve a 2x reduction in safety. This looks consistent with recently released data from train passengers sitting directly adjacent to one another versus merely in the same row (Hu et al.). If you’re breathing right into each other’s faces, more so than train passengers would, maybe use a higher number.
We think it doesn’t make sense to take the full “outdoor” bonus when cuddling, because your faces are very close together. Finally, we think a brief hug probably doesn’t meaningfully change your risk, but we don’t have any evidence for that. Basically, we really don’t know and don’t have any evidence here, so take this with more grain of salt than the rest of our more-research-backed numbers.
A one-time hangout combined with the kissing multiplier is an Activity Risk of 5 ⨉ 14% per hour = 70% per hour, which can be capped off to the live-in partner multiplier of 60%. As a side note, it seems to us that masked sex might be a lot safer from a COVID standpoint than making out without masks... provided you actually have the willpower to keep your masks on!
Cuddling and hugging aside, is it risky to touch the other person if we remain a normal socializing distance apart?
We don’t feel we have enough data to fully model this risk. But if we assume you aren’t changing how far apart you are, then we think that hand-to-hand touching is more risky than other kinds of touch. Any type of touch is safer if you wash or thoroughly sanitize your hands both before and after touching.
If you’re within hand-holding distance of someone, and you reach out and touch their hand, it does not change your chance of inhaling a respiratory droplet, because your faces didn’t really move. What does change is the chance that any virus that’s on their hands (from rubbing their nose or coughing) could get from your hands into your eyes, nose, or mouth (when you touch your face). Touching hand-to-hand seems likely to be riskier for this route than other types of touch (such as clasping forearms, giving a shoulder massage, or a brief hug with faces averted).
The CDC says that contact transmission is not a main driver, but we haven’t yet seen research on this topic we feel we can trust. For our house, we’ve learned to treat our hands as “contaminated” any time we’re outside the house, and to wash our hands as soon as we get home. As such we don’t currently add an extra budget factor for touching or not. You could perhaps assume that touching bare hands adds another 2x factor (which is as much as we use for cuddling) if you expect you won’t manage to wash your hands before touching your face, but we’re entirely making that up and we don’t use it in our estimates. We don’t have a better suggestion we can stand behind right now.
Touch is a psychologically powerful way to show affection and appreciation. In our experience, outdoor masked hand-holding has a huge positive impact on our mental health and feeling of connection, as compared to assiduously not touching one another. Feeling “touch starved” is a real thing with real psychological effects, and for many people we think touch is a good use of your risk budget.
How do I count receiving a package?
We don’t currently count microCOVIDs from packages, because of our understanding that fomite transmission is not a primary driver of the spread; most of our risk comes from time we spend indoors with others. People maintaining much lower annual risk levels than us might prefer to sanitize packages to maintain a stricter risk tolerance.
Health officials are often quoted as saying the risk from packages is “very low” and “unlikely,” but until they quantify that in microCOVIDs we’re just going to proceed with assuming it’s less than 1 microCOVID per package. We do know there’s no known evidence of transmission from food packages.
Lyfts/Ubers?
You’re indoors, about six feet (two meters) away from one other person (the driver), and both of you are hopefully wearing masks. It’s an unusually tiny space with poor air circulation by default.
We did some informal tests with a CO2 meter in a Lyft[7], and found that if you crack the windows open by an inch or so, this makes it “just” as well ventilated as a normal indoor space, rather than much stuffier than usual. So we suggest to at least crack the windows, then count it like an indoor space. If they’re chatting or talking on the phone, you might consider politely asking them not to.
If you keep the windows all the way open, the air circulation according to our CO2 meter is just about as good as being outdoors, so you’ll probably reap some of the benefits of being outdoors. We wouldn’t recommend taking the full 10x outdoor modifier for a windows-open Lyft, since it’s unclear how much of the safety of outdoor interactions is due to factors like UV light that aren’t present inside a car. But 2x or so might be reasonable.
Public transit?
You can very conservatively treat transit as an indoor hangout with however many other people are in the bus or train car with you, continuing to take a decrease of 2x per additional 3 feet (1 meter) away that the people are. You’re also probably up to 5x safer in the likely event that nobody is talking (but if anyone starts yelling, which happens on public transit sometimes, you could be 5x less safe). Overall, very few transmission clusters have been linked to public transit.
Airplanes?
Unlike transit, airplanes have pretty good air filtration systems: all the air is replaced with new air from outside every 4–5 minutes, and all the air passes through a HEPA filter that eliminates 99.97% of particles (the same as a P100 respirator) every 2–3 minutes (source). That means your risk will primarily be from people near you.
The exact numbers for the Activity Risk will depend on how full your flight is; we’ve used 20 people at 6 feet (2 meters) of distance as a reasonable estimate for a moderately full flight. The worst case of a middle seat on a totally packed flight might be twice as bad as that:
- Two people right next to you: potentially equivalent to about 8 people six feet (two meters) away (though there’s a lot of uncertainty about risk at extremely close quarters)
- Six people in the rows ahead of you and behind you, about 3 feet (1 meter) away: equivalent to about 12 people six feet (2 meters) away
- 21 other people within two rows of you (five full sets of 3 seats across the aisle, one that’s two rows ahead of you and one two rows behind), all of which are about six feet (two meters) away which adds up to 41 people. (The plane is divided into “zones” of 5–7 rows each with separate climate control systems, so 5 rows worth of people — yours, two in front of you, and two behind — is a pretty good estimate for how many you’re potentially sharing exhalations with). As with public transit, you probably get some benefit from the fact that few of the people around you are talking, though it’s hard to say how much. Anything you can do to reduce the number of people near you (such as flying at an inconvenient time, paying for a reserved or extra-legroom seat, or even buying a first-class ticket) will help reduce your risk.
For the Person Risk, we suggest you use the maximum prevalence of your source or destination region.
What about the airport rather than the plane? We still suggest you wear a high-quality mask. However we also note that airports are huge spaces and at the time of writing we’re still at only about 20% of the passenger volume per day compared to what we saw last year—with decreases in demand, the flights get fewer but the airports don’t get smaller. It’s also easier to distance in the airport. Our intuition is that most of your risk comes from the plane.
Overall, there are very few documented cases of transmission on airplanes, which is surprising given that 500,000 or more Americans are flying every day at the time of writing (which, if we naively assume current US-wide prevalence rates, would mean ~100 COVID-positive passengers per day). We are aware of one flight in China in January 2020 that infected 12 people, one case in February probably acquired on a flight, and one flight in March from London to Vietnam that infected 13 people. Erin Bromage has written more on flying in the age of COVID-19.
Grocery stores? Drug stores? Haircuts?
For grocery stores, we count the average number of people near us: in our neighborhood this is usually about 5 people, keeping 6 feet (2 meters) away, everyone wearing masks. For drug stores, pharmacy pickup, or medical buildings, you might want to add an extra boost to Person Risk to account for the fact that the people you’re encountering are more likely than average to be sick.
Haircuts can be modeled by counting each person in the hair salon. We definitely recommend wearing the best mask you have that won’t interfere with the haircut, and checking in advance that your mask style will be fine. If your stylist is usually chatty, we suggest for an extra safety margin to ask the hair stylist to chat less! We found an anecdote on Twitter about 140 clients who were in close contact with two infected hair stylists, indoors, with both client and stylist wearing masks. 45 clients were tested – all negative – and we haven’t heard of any cases among the others. Last we checked this was statistically consistent with the Activity Risk and modifier suggestions we use in this writeup.
Going to a protest?
Warning: This answer hasn't been updated for the Delta variant.
The risk of attending a protest depends on how close you get to others, whether they are yelling/chanting, whether they are wearing masks, and other factors we have not modeled in this writeup (for example, we have heard anecdotally that it is lower risk to be in a group where people are moving constantly, rather than staying near the same people for a long time). If you are in a shoulder-to-shoulder group of yelling people without masks, you might be near 10 people within 6 feet (2 meters): Activity Risk = 6% per hour ⨉ 10 people ⨉ (1/10 outdoors) ⨉ 5x yelling (see earlier in Q&A) = 30% per hour. Alternately, if you are in a group of cyclists protesting by biking down the road banging drums and gongs, that might be more like Activity Risk = 6% per hour ⨉ 10 people ⨉ (1/10 outdoors) ⨉ (1/5 silent) ⨉ (1/2 at least 6ft away) = 0.6% per hour. This is a 50 times less risky activity. There are many ways to protest. We encourage you to keep all the same heuristics in mind: if possible, avoid very dense crowds, yelling, and enclosed spaces; and wear masks to protect yourself and others.
The most important thing to remember in attending a protest is that you may not have control over what happens to you. Police might pull your mask off. If pepper spray is used, people are likely to cough uncontrollably. You might get kettled into a small area, even if you were planning to keep your distance from others. One thing you can do to help stay safer is to make a plan in advance about what you will and won’t do: for example, you might decide in advance that if you see any gas used near the protest, you will leave. By thinking about what you are and are not up for, and making choices that take into account the risks, we hope you can confidently and proudly participate in protests that make sense for your risk tolerance.
Related Work
How do microCOVIDs relate to initial dose?
"Initial dose" — sometimes referred to as “initial viral load” — refers to how big a “dose” of virus you get when you first get exposed to the virus. If you’re exposed to more viral particles, evidence suggests that you’re more likely to develop a severe infection. This means it’s important to try to reduce the strength of your initial exposure, not just in order to avoid getting sick.
For the same total number of microCOVIDs, our guess is that getting them from many smaller independent sources (many mask walks, numerous brief grocery runs, etc.) is more likely to involve a low initial viral dose than getting them from fewer riskier contacts (household members who don’t take many precautions; cuddling a random person whose recent activities you don’t know).
Are there other similar models or scales?
Here are some quantitative analyses we like:
- Peter Hurford of Rethink Priorities created a COVID Risk Calculator which we really like. His approach is entirely compatible with ours, although he uses some different numbers. The tool outputs a risk of COVID infection in terms like “1 in 578” which is easy to convert by multiplying by a million to e.g. 1730 microCOVIDs
- Prof. Jimenez from Univ. of Colorado-Boulder has an aerosol transmission estimator in a Google Sheet that informed many of our numbers. Unlike our analysis, this sheet uses detailed assumptions about the dynamics of particles in the air. Each tab gives a risk of infection for a specific scenario.
- The NYTimes has an easy-to-digest discussion of COVID risk in terms of micromorts.
In terms of qualitative scales, we like the following:
- The interactive guide at COVID - Can I Do It?, where you can plug in an activity and see its risk breakdown in terms of crowding, respiratory droplet formation, time, and ventilation.
- The diagram of red/yellow/green activities by Popescu et al. which was featured in a FiveThirtyEight article about risks and decisionmaking.
The data from the study are truncated at 130 days (~18.5 weeks), at which point 12% of the study participants infected with COVID continued to experience symptoms (Figure 3 from Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 1 April 2021). ↩︎
More concerning symptoms include cough, chest tightness/discomfort, obvious sore throat, body aches, malaise, loss of taste/smell, nausea/vomiting, loss of appetite, diarrhea, any subjective “feverish feeling” or elevated temperature, fainting, or thermometer reading of >100.4. ↩︎
You probably can't do this anywhere near as reliably with someone you don't live with, which is why the discussion here is specific to housemates. ↩︎
Perhaps a lot less likely that I get it from Alice if Alice isolates promptly: Li et al. found that isolating an infected household member from the rest of the household as soon as they showed symptoms was effective in all the 105 cases they studied at preventing anyone else in the household from getting sick. ↩︎
This is due to the fact that much less transmission occurs more than 3 days before the appearance of symptoms (He et al, figure 1c middle graph) or fewer than 2 days after infection (Ferretti et al, figure 1 “generation time”). In order for Carol to infect Bob before Alice shows symptoms, Carol’s generation time would have to be greater than the delay between Alice’s infectiousness and Alice’s symptoms, which is unlikely. ↩︎
When we do these calculations, the lowest Person Risk we allow ourselves to assign anyone is 1/100th the Intermediate Person Risk, just as a safety margin. ↩︎
Jimenez’s aerosol transmission tool lends some support to the idea of using CO2 as a proxy for density of exhalations. ↩︎
Research Sources
Read this section if you are interested in the epistemic nitty-gritty behind our estimates of Activity Risk and Person Risk.
Activity Risk
Indoor unmasked transmission
One-time contact
This is the chance that you would get COVID from spending more than 10 minutes indoors or in close proximity to someone who is COVID-positive. We estimate this as "about 14% per hour."
For the original virus, we estimated “about 6% per hour” from combining multiple sources:
- In a study of train passengers that analyzed 2,334 index patients with COVID, Hu et al. found that passengers on seats within the same row as the index patient had an average attack rate of 1.5%; for passengers in adjacent seats, the attack rate increased 1.3% per hour. Assuming train passengers are mostly silent, combining this with the respiration rates from the Jimenez Aerosol Transmission Model would imply that a conversational hangout in the adjacent seat of a train would be a risk of roughly 6% per hour. The distance between adjacent seats on this train was half a meter, and we think typical socialization is moderately further away than this, which gives some extra breathing room on the estimate.
- Using the Jimenez Aerosol Transmission Model, we modify the “Class” scenario (1 infected instructor speaking loudly) to propose a normal conversational volume, smaller room (10ft wide x 14ft long x 10ft high), and no masks, leaving other parameters unchanged. This outputs 2.8% per hour; however, this model notes it assumes uniform mixing of air and ignores near-field effects, so is not a good estimate for interactions that aren’t 6+ feet (2+ meters). If we take this as our 6+ feet (2+ meters) estimate, and double it as per the “Distance” modifiers described later, this also suggests 6% per hour. (Note that this is rather dependent on room size: increasing the 10ft width to 15ft decreases the estimate by a third.)
- Bi et al analyzed Shenzhen contact tracing data from Jan 14–Feb 12 (1281 contacts of 291 cases). Their Table 3 provides data about how often close contacts of COVID-positive people got infected based on different types of contact. The average estimates for each group tend to fall roughly between 6-9% (total, not per hour); we note that the vast majority of the infections in this dataset come from the “Contact frequency: Often” category, so we expect this to be an overestimate for the “Moderate” and “Rare” frequency. This data was collected in a setting where 17% of cases were isolated before symptom onset, and we would expect a larger fraction isolated after symptom onset, so the numbers would be higher in a setting where people are not being notified when their contacts get sick.
- Next is Chu et al who did a meta-analysis of 172 studies covering 26,000 individuals, to determine the impact of various interventions (masks, distance, and eye protection) on transmissibility. Importantly to note, they included analyses of SARS and MERS, not just COVID-19. As shown in their Table 2, they found baseline transmissibility values (without masks/distance/etc) of 12.8%, 17.4%, and 16% in different groups. These data mostly come from healthcare settings, and the baseline assumption is direct physical contact, rather than an ordinary socializing distance. We don’t know how many hours were generally spent with patients. We assume these are infected patients who have sought treatment, so definitionally there is no additional distance from anyone symptomatic, so we might expect casual social contact outside a healthcare setting to carry a lower infection probability. However, COVID-19 may be more infectious/contagious than SARS and MERS. Overall, this is consistent with “6% per hour” for normal socializing if the average duration in this dataset is on the order of 2 hours; if the baseline “no distance” is closer together than typical socializing; or some combination.
- In a prospective study in Taiwan, Cheng et al found a secondary attack rate of 1.0% among contacts of longer than 15 minutes who were exposed within the first 5 days of symptom onset. This implies a rate of 4% per hour if all the contacts were only 15 minutes (and even lower rates if the contacts were for longer).
When B.1.1.7. became the dominant variant, we increased this number by 1.5x based on Davies et al which found that a 56% faster growth rate best explained the rapid expansion of the B.1.1.7. variant vs other variants.
When Delta became the dominant variant, we increased this number by 1.5x again based on Allen et al. finding 1.6x the number of secondary transmission clusters in households which had an index patient infected with the delta variant vs households where the index patient had been infected with B.1.1.7.
Household member
This is the chance of getting infected from a household member who has COVID. We use the estimate of 40%, which we get via a naive analysis of the data in Allen et al., which is, to our knowledge, the only study of household tranmission with the Delta variant.
We note that this is only 1.3x the original transmission risk for households members. This could indicate that the original number was too high, or it could indicate that households are becoming better at isolating infected individuals, driving down the overall chance of household transmission.
Previously we used 30% from the meta-analysis of Curmei et al. (specifically their updated June 27 version). We explain a bit here about where their estimate comes from.
Curmei et al. used three different methods to synthesize existing literature. The first method is a re-analysis of nine recent studies, which gives them the central estimate of 30% for the “secondary attack rate” (which is the parameter we care about: the chance of getting infected from a housemate who has COVID). They point out that the estimates vary substantially from source to source, which they conjecture is likely in part due to variations in isolation practices.
Their other two estimation methods use independent datasets. Although these two methods don’t estimate secondary attack rate—rather, they estimate Rh, the number of within-household transmissions, which is not quite the number we’re looking for—we can nonetheless use this information as corroboration. Specifically, they estimate an Rh of 0.37 from Vo’, Italy, where average household size was 2.1. If the average infected person infects 0.37 of their 1.1 (excluding self) other household members, that works out to each household member having a 34% risk of being infected. The data suggests this could be substantially larger for older people.
Partner
This is something of a speculative number. We found two studies that compare household transmission among spouses vs non-spouses:
- Li et al. found a 1.6x higher transmission rate among spouses than among other adult household members.
- Lewis et al. found a 1.4x higher transmission rate.
We use this to adjust the 40% figure from Allen et al. up by 1.5x, to get ~60% for spouses.
This number was updated from 48%[1] to 60% as part of the Delta variant overhaul in July 2021.
Modifiers to Activity Risk: Masked, Outdoors/Ventilation, Distanced
Masks
Note: we updated our mask categories and numbers in late January of 2021.
We divide our analysis into protecting others (source control) and protecting the wearer (PPE). We draw the majority of our sources from the Howard et al. Evidence Review (version 4 from Oct 2020), which surveys a variety of study types, some COVID-specific, and some studying particle filtration as a property of the fabric, or for other pathogens such as influenza.
Masks: Protecting others
For protecting others (i.e. source control), we draw on the following sources, three of which are new in this revision of our estimates:
- Davies et al.: percent filtration of influenza microorganisms isolated from coughs, and total reduction in colony-forming units.
- Milton et al.: proportion of flu viral copies reduced vs no mask on patient.
- Fischer et al.: relative droplet count as show in Fig 3
- Kumar et al.: simulation of leakage and airflow
- van der Sande et al.: protection factor from inside to outside (concentration ratio)
- Lindsley et al.: proportion of cough aerosol blocked
- O'Kelly et al.: fit of different mask types by untrained volunteers
We start by estimating a number for surgical masks specifically. The below table shows the various results from these studies:
| Source | Measurement | Outcome |
|---|---|---|
| Lindsley et al. | Proportion of cough aerosol blocked | 60% (1.7x reduction) |
| van der Sande et al. | Protection factor | 2.5x |
| Milton et al. | Reduction of viral copies | 3.4x |
| Reduction of "fine" aerosols | 2.8x | |
| Reduction of "coarse" aerosols | 25x | |
| Davies et al. | Reduction of colony-forming units | 7x |
| Kumar et al. | Proportion of airflow that leaks around mask | 12% (8x maximum protection) |
| Fischer et al. | Reduction in droplet count from coughs | 10x |
We conclude that surgical masks are significantly better at blocking large particles (25x) than small ones (2.8x) Milton et al.. It appears that coughs are filtered very effectively [Davies et al.], [Fischer et al.], which seems to imply that they are predominantly large particles. Thus, we chose a number slightly higher than Milton et al's overall number (3.4x), which is 1/4.
For masks that provide less protection to others, we derive our estimates for thin and thick cotton masks by using relative comparisons to surgical masks and to one another. Davies et al. Table 1 shows that a "scarf" is about 56-65% as protective as a surgical mask, and a "cotton mix" is 70-78% as protective as a surgical mask. Davies et al. Table 4 suggests that the homemade mask was about 92% as effective at blocking colony-forming units as a surgical mask. Fischer et al. shows the relative droplet count in Fig 3 for "bandanas" as 0.5, and for "cotton" as 0.2 (i.e. 80% of droplets filtered), implying a bandana is about 60% as effective. Finally, the Lindsley et al. proportion of cough aerosol blocked is 47% for polyester neck gaiter and 60% for a procedure mask (which we think is a surgical mask), implying a neck gaiter is 78% as effective as a surgical mask. Overall, in summary, we interpret these ratios as implying that a thick, well-fitted cotton mask would be about 80%-90% as effective as a surgical mask (which we estimated above reduces others' exposure by 4x), which makes 2.5x-3x protection which we round off for simplicity to 3x (1/3 multiplier) for thick cotton masks. In turn, a thinner or worse-fitting homemade mask looks to be no less than 50% as effective as a surgical mask, which we round off to 2x (1/2 multiplier) for thin masks or worse fit.
We didn't find any sources describing fitted masks with PM2.5 filters. We choose to guess that these are more protective than thick fitted cotton masks, and about as protective as a surgical mask due to similar fit characteristics and similarly being made from a fabric whose filtration properties were considered in the design, so we suggest the 1/4 multiplier for masks with PM2.5 filters.
For masks that provide more protection to others, such as KN95s and N95s, we make a distinction between getting a truly airtight seal, such that all the exhaled air is going through the mask, versus just wearing a rated mask on one's face without being sure it has sealed, allowing for some leakage.
Despite the fabric often being highly rated for filtration, KN95 masks usually provide a loose fit, with visible gaps, roughly in the same ballpark of fit as a surgical mask (O'Kelly et al.). In our personal experience with earloop KN95s, we have not been able to get a firm/tight seal. We therefore would estimate their protection factor as being in roughly the same 1/4 ballpark as surgical masks (not in the rated ballpark of 95% protection i.e. 1/20 reduction), but perhaps slightly higher due to improved fabric and somewhat improved fit. To quantitatively estimate the amount of improvement, we extrapolate from Mueller et al. who estimate how much better "cone-shaped" masks such as KN95s tend to fit than surgical masks, although their study was on protection-to-wearer rather than protection-to-others. They show about 10% better filtration performance (Fig 7B), which implies a slightly-improved 1/6 factor for KN95s as contrasted with the 1/4 factor for surgical masks. We note this is a fairly speculative estimate, as the data on KN95s is limited. We also use this estimate as the protection-to-others factor for an N95 mask that the wearer has NOT checked for a seal.
For a NIOSH-rated medical-grade N95 mask that the user has checked for an airtight seal (No outflow valve; No beards; No earloops, elastic headbands needed for tight fit) we don't find any studies measuring real-world source control properties, because most studies assume these masks are worn for PPE. Some studies already analyzed earlier in this section suggest extremely good protection to others from an N95: Fischer et al. shows an incredibly small relative droplet count, below 0.001, as show in Fig S1; Lindsley et al. shows a 99% proportion of cough aerosol blocked. for N95 respirator. We assume therefore that sealed N95s provide very good protection, although we are reluctant to assign values higher than the NIOSH-rated 95% (1/20). To get to our final figure, we draw on the broad trend we observe in comparing protection-to-others factors (this section) with protection-to-self factors (next section) for the lesser-rated masks: across the board, we estimate approximately a 2x larger protection-to-others factor compared to the protection-to-self factor for the same mask type. Therefore, we start with a PPE analysis of well-sealed N95s (below), which estimates a 1/8 protection factor worn as PPE, and extrapolate a twice-as-good 1/16 protection factor for well-sealed N95s worn to protect others.
Finally, when wearing a reusable P100 respirator with the outflow valve covered with fabric, we assume the same effect in protecting others as a fabric mask: 1/3. This is a guess; the data behind the 1/3 estimate assumed some amount of "leakage" whereas a fully covered valve is more likely to direct all the exhaled air through the fabric, which might suggest more outgoing protection; however, the exhaled air emerges in a more concentrated "jet", which might suggest less protection. We don't have a good way of knowing, so we go with our best guess.
We note that in a more nuanced analysis we might consider estimating a smaller protection factor at further indoor distances, and a larger protection factor at close distances, because surgical masks are particularly effective at stopping droplets (Leung et al.) which travel shorter distances. However, for ease of use, the microcovid model makes an independence assumption of the various mitigating factors and variables.
Masks: protecting the wearer
For wearer protection (i.e. PPE), we draw on the following sources, five of which are new in the latest revision of our estimates:
- Mueller et al.: percent removal of particles from outside to inside of mask
- van der Sande et al.: protection factor from outside to inside (concentration ratio)
- Konda et al.: filtration efficiency of fabrics
- Zhao et al.
- Offeddu et al.: review and meta-analysis of healthcare workers
- Chu et al.: meta-analysis
- Liang et al.: meta-analysis.
- Lai et al.: mannequins with aerosol spray
- Gardner et al.: P100 respirator performance against infectious airborne viruses
As with the protection-to-others estimates, we start with surgical masks. A handful of sources cluster around approximately a 2x protection factor ballpark, including Offeddu et al. estimating 60% protection against respiratory illness in general, and 34% against flu; Chu et al. estimating 2-3x protection (although as Howard et al. observe, they put substatial weight on SARS and MERS results); Liang et al. estimating that high-quality masks worn by non-healthcare-workers give 47% reduction; and Lai et al. showing in Figure 5 (black vs. pink curve) an approximately 60% reduction in concentration at the mask-wearer's mouth under conditions of normal wearing. Additionally, Konda et al.'s filtration efficiency of surgical mask fabric with a gap reported at 50%. Some results appear higher, including multiple measurements in the van der Sande et al. paper that are in the 4x ballpark (see Table 1), and the Mueller et al. results showing 53%-75% particle removal. Some results come in lower, such as Zhao et al. estimating only 19-33% of particles blocked even with a tight seal. Overall we feel that 1/2 wearer protection from surgical masks is an adequate summary of the data.
For durable cloth masks that fit well, we draw on the following sources: Mueller et al. shows particle removal in the range of 28%-91% from a well-fitting cloth mask; Konda et al. show filtration efficiencies from 2-layer cotton in the range of 38%-82%; van der Sande et al. measure a protection factor of 2.5x. Overall, it seems that some cloth masks achieve comparable efficiency to a surgical mask, but there's substantial variance; since the lower end of the range is in the 30% ballpark, we feel comfortable suggesting a 2/3x multiplier to the wearer from a thick and well-fitted cotton mask.
For thin, light materials and poor fit, we did not find any evidence suggesting substantial protection to the wearer. Konda et al. suggest only 9% filtration from a quilter's cotton fabric. We suggest no protection, a 1x multiplier, to the wearer from thin or loose-fitting masks
For KN95 protection-to-wearer, we use the same data from Mueller et al. about cone-shaped masks showing they are an improvement over surgical masks but not drastically so. Additionally we draw on Lai et al. showing that a face mask that is sealed on three sides (but open on the fourth) is about 60% protection, which leads us to think that a 1/3x multiplier from a cone-shaped KN95, as compared with a 1/2x multiplier from a surgical mask, is a reasonable estimate.
For well-fitted and well-sealed N95 masks (no outflow valves, tight-fitting elastic headbands, and no beards) we draw our number from Offeddu et al.. In Fig 5C, they show a number of studies that found a risk ratio of 0.12 between healthcare workers who wore N95's while working with SAR-COV-1 patients and healthcare workers who wore no mask. This represents an 88% relative risk reduction, or a multiplier of 1/8.
We note that Offeddu et al, along with several other papers including Long et al. and Radonovich et al. found lower effectiveness at N95 masks reducing the rates of influenza among healthcare workers. We note (as do several of these papers) that these studies are unable to determine whether the workers were infected by patients or by normal community spread; all of the infection rates fall well within average population rates for influenza. Thus, we consider these studies underpowered for determining efficacy of PPE.
In our original writeup, we cited that Chu et al. finds a difference between N95s (adjusted odds ratio of 0.04) versus other masks (adjusted odds ratio of 0.33) in contracting diseases such as SARS and MERS that workers were unlikely to contract in their daily lives.
As a sanity check, we offer several studies that test the filtration characteristics of N95 masks:
- Mueller et al. showed 90% of small particles were blocked (less than 0.3 micron);
- Zhao et al. showed 95% blocked;
- Konda et al. showed 85% protection with no gap;
- van der Sande et al. show multiple measurements above 85x (!) protection;
- Lai et al. show that the protection from a fully-sealed mask is >89%, and drops to >80% with small leakage.
Overall, Offeddu et al. is the most compelling study, so we use a factor of 1/8x, acknowledging that this could be as little as 1/5x (80% filtration) if there is some leakage, or as much as 1/20x (95% filtration) in cases of perfect usage.
We note this is slightly less than the Respirator assigned protection factors for this type of PPE, explained in more detail in the next paragraph.
Estimating the wearer protection from a resuable NIOSH-approved P100 respirator requires looking beyond the infectious disease literature, as these types of respirators are seldom worn in healthcare settings or studied in real-world protection from infectious disease. Gardner et al. show in controlled conditions that P100 respirators met or exceeded their rated 99.97% filtration efficiency in filtering out viral particles in an aerosolized liquid suspension, so we do not doubt that P100 masks are fully as protective against viral aerosols as they are against other contaminants. The question that remains is what the real-world likelihood is of an untrained person getting a perfect seal. For this, we defer to standardized Respirator assigned protection factors (APFs), which convert rated filtration efficiencies to the expected real-world decrease of the concentration of inhaled contaminants, based on studies in the workplace. For our P100 estimate, we choose to use the higher protection value of 20x from the UK FFP3 mask, rather than the 10x value used in the US, because the US value is assuming a truly grueling "worst case" - work in the polluted atmosphere of 8 hours per day, 40 hours a week - and we assume calculator users are not intending to wear P100s for this duration.
One note is that we are additionally drawing on our personal experience in feeling comfortable recommending a higher protection factor for P100s than for N95s, because in our experience helping friends get a seal on their mask, it is vastly easier for an untrained person to get a reusable P100 respirator to seal well on their face than it is for them to get a seal on an N95, even if it is the right shape and size for their face which is far from guaranteed.
For users seeking even higher protection than 1/20, we suggest eye protection, including full-face masks, as described in the Respirator assigned protection factors wikipedia page.
Outdoor / Ventilation
Outdoor
This is one of the tougher numbers to estimate, but we currently feel good estimating that being outdoors reduces your risk by more than 20x (unless you’re super close together, in which case we’re really not sure).
Almost every news article about outdoor transmission cites the same two sources: Nishiura et al. and Qian et al. Nishiura et al. is the source of the “18.7x” figure that we see all over the place, but we don’t put much stock in this specific paper for two reasons. For one, many summaries seem to miss that this is an odds ratio and not a relative risk ratio (that is, it tells us that 18.7x as many of the transmissions came from indoors, but if people in general usually had 18.7x as much indoor contact as outdoor contact, this would not imply any difference in risk!).[2] For another, Nishiura et al. also uses a very small sample size, it’s only six scant pages with very little explanation, and we can’t make heads or tails of the bar chart at the end.
Instead, we put stock in two sources:
- Qian et al looked at 7,324 identified cases in China, and only found one outdoor outbreak involving two cases (which we interpret as one primary case, who had a conversation with the secondary case). Americans spend about 8% of their time outside; if we assume the same holds in this population, and close contact follows the same distribution, and there was no difference in indoor and outdoor risk, then this would imply 629 outdoor cases in expectation. A factor of several-100x lower risk needs to be accounted for somehow, through some combination of reduced outdoor risk and overestimating number of outdoor contacts.
- Professor Jose Jimenez’s Google sheet Aerosol Transmission Model[3], which is one of our absolute favorite resources so far. Professor Jimenez models the Skagit Choir outbreak, and then re-does the model again as though the choir had been outdoors, and finds transmission rates 100x lower outdoors. Notably, this model does NOT include the contribution of larger respiratory droplets, and assumes 6ft social distancing.
There’s also anecdotal evidence. In addition to the reports that there was no significant protest-related surge as a result of the Black Lives Matter protests, we also heard from a friend of ours who took a CO2 meter to a crowded protest and observed that the CO2 readouts were totally flat, implying minimal density or buildup of exhalations.
Finally, there have been zero outdoor outbreaks of any kind in the US, whereas in Colorado 9 percent of outbreaks are reported to have been traced to bars and restaurants, despite the fact that both indoor and outdoor restaurant dining are open throughout the US.
The sources above hint at up to a 100x benefit. Fellow armchair modeler Peter Hurford assumes a 5x benefit from being outdoors. We feel good about calling it “more than 20x” for now and waiting for more evidence, with a warning about not trusting this number if you’re very close to one another because we have no data about outdoor cuddling.
Ventilation
We draw our figure for room with HEPA filters from Curtius & Schrod, who found that running HEPA filters in a class room with total hourly flow rate equal to 5x the volume of the room to decrease the concentration of aerosols in the room by 90%. They further project that this would decrease the liklihood of COVID transmission by 3x for a 1-hour interaction and 6x for a 2-hour interaction. We split the difference apply 4x in the calculator (but note that the longer your interaction lasts, the greater an impact air purifiers will have). We note that simply circulating air is insufficient - the air must either be exchanged with the outside or passed through a high quality filter (HEPA is equivalent to P100; HVAC filters rated on the MERV scale do not meet this critieria.)
It's important that your filter is actually circulating sufficient air.
- Look up the model of your air purifier online; it should have a rating in CFM, which will be for running at maximum.
- Measure the length and width of your room in feet.
- For a normal room height (8ft), ensure
CFM > 2/3 * length * width
The derivation of this rule is as follows:
Refreshes/hr = 60 min/hr * CFM ft^3/min / (length ft * width ft * height ft) = 5
60 * CFM / (length * width * height) = 5
CFM = 5 * (length * width * height) / 60
CFM = 1/12 * (length * width * height)
if height = 8ft,
CFM = 2/3 * (square footage)
From this, we also deduce that areas that have high rates of air exchange while not being "outside" per-se should be similarly safer. This includes cars with the windows rolled down and partially enclosed spaces (i.e. at least one wall is open to outside air).
Finally, many mass transit options have very high air circulation standards, so we apply the same risk reduction. For instance, SF's BART claims that their trains circulate and purify air every 70 seconds, or 50 times an hour.
On planes, Silcott et al directly measured aerosol concentrations on a plane and found that the plane's filtration system resulted in 90% less exposure than a house. Since this is the same reduction as Curtis & Schrod found, we reason that the same reduction should apply. However, plane rides tend to be 2+ hours, so we use the 6x reduction that Curtis & Schrod calculated.
Distance
This is another Chu et al estimate. Each meter of distance was associated with about a 2x reduction in infection risk; specifically they find that being one meter apart is 2x better than baseline, and two meters 2x better than one meter. They speculate, and we agree, that three meters is thus likely at least 2x better than two meters. Although these data come from a healthcare setting in which “0m” means direct physical contact with the patient, we instead conservatively take “baseline” as “normal socializing” ≈ one meter. When doing our own personal risk calculations, we estimate “cuddling” = zero meters as twice as risky as baseline.
We get some corroboration for this number from the study of train passengers, Hu et al. Looking for example at Figure 3, for passengers that were 1 row apart, moving an additional 2 columns away (seats 0.5m wide, so about 1m away) decreased the risk from what we eyeball as 0.2ish to 0.1ish, and then from 0.1ish to 0.05ish for an additional 2 columns. It’s worth noting that they report a steeper drop from sitting right next to the index patient to sitting 1m away, which could be relevant to hangouts at closer than a normal social distance from someone.
Person Risk
Basic Method: Underreporting factor
Previously we rolled out own estimation of underreporting factor based on raw caseloads. We now follow the model buit by COVID-19 Projections. Their team fit a model to seroprevalance data from various points in the pandemic.
The model they use is:
 This model works on the assumption that testing availability has steadily improved over the course of the pandemic, such that the impact of the positive test rate decreases as the pandemic continues. Our original model was based on a snapshot of testing availability early in the pandemic, which is now overly pessimistic.
This model works on the assumption that testing availability has steadily improved over the course of the pandemic, such that the impact of the positive test rate decreases as the pandemic continues. Our original model was based on a snapshot of testing availability early in the pandemic, which is now overly pessimistic.
For historical purposes, here is the original model that we used:
In order to make suggestions about underreporting factor, we threw together a quick comparison of two data sources.
- The first data source is state-by-state historical Positive Test Rates from Covid Act Now.
- The second is the CAR (case ascertainment ratio) columns of this table from the NIH, as explained in Chow et al. (which used a computational model to estimate these numbers).
- We typed these in by hand hastily. We excluded the NY and NJ numbers as the two that did not have a specified Positive Test Rate, being listed just as "over 20%", in the relevant timeframe. If you would like to check our work, this code snippet shows what we did.
There was a visible correlation, so we eyeballed some approximate ranges. Here's the data we see, with a simple linear regression line drawn on top. We eyeball this as being roughly "1 in 6" on the left-hand side; "1 in 8" in the middle; and "1 in 10" on the right-hand side.
Contagiousness adjustment
The way we're using the prevalence numbers in our model assumes everyone in your area with COVID is equally likely to give it to you. But in reality, that's probably too pessimistic:
-
A high proportion of all cases are asymptomatic. There's some uncertainty about the exact fraction, but a literature review by Oran et al. estimates 40-45%.
-
Asymptomatic cases are less likely to ever be tested than symptomatic cases, because symptoms prompt people to get tested. In the absence of symptoms, you'll only know you have COVID from contact tracing or from an effectively "random" / "just to be sure" test. This implies that asymptomatic cases are likely to be a relatively smaller fraction of reported cases than of all cases.
-
Asymptomatic cases are probably responsible for quite a low proportion of infections. Ferretti et al. concluded that only 5% of infections were caused by someone asymptomatic (i.e., who will never show symptoms no matter how long you wait).
-
Our data about transmission likelihood (Activity Risk) are probably drawn from mostly symptomatic index cases. Thus, asymptomatic cases are likely to be less risky than our model would indicate.
In a region with positive test rates below 5%, we estimate the number of infected people as 6x the number of reported cases. But if reported cases are relatively more likely to be symptomatic, and unreported cases relatively less so, and asymptomatic cases are less risky in terms of onward transmission... then there's an argument that just multiplying the number of reported cases by 6 is too pessimistic. Even if the number of infections is 6x the reported case count, the risk to you would be lower since so many of those cases are asymptomatic. Maybe the increase in risk due to those unreported infections is only 4x or 5x, even though the underreporting factor is 6.
We can make a fairly speculative guess at what this "contagiousness-adjusted" underreporting factor should be, as follows. Testing provider Color observes that 30% of their positive test results do not have any symptoms at the time of testing, and thus we infer are either presymptomatic or asymptomatic. If we again use the ratio from Oran et al., we might guess 40% of those 30% will never show symptoms; which is to say, we guess 12% of all Color-reported positive tests are from asymptomatic cases, and the remaining 88% are from presymptomatic and symptomatic cases. By contrast, 60% of all total infections found via blanket testing of everyone in a region (by Oran et al. again) are presymptomatic or symptomatic. This tells us that we might expect 0.6/0.88 = ~2/3 as many of the unreported cases are highly contagious (by virtue of being presymptomatic or symptomatic instead of asymptomatic). While this calculation is far from perfect, it gives us a rough estimate that could be used as a "contagiousness adjustment factor" of 2/3. And that would imply that the minimum underreporting factor could be 4x, not 6x.
We have chosen not to apply this adjustment to the estimates we report in the main text: the underreporting factors of 6x/8x/10x assume all cases are equally contagious. We made this choice because of how speculative the adjustment is. Even though we're reasonably sure from first principles that there should be some effect along these lines, we're quite uncertain about its magnitude. So, we'll treat the effect as an unknown safety margin rather than using it to reduce our prevalence estimate.
Infectious period
We state in the Advanced Method that a person’s risk is the sum of all of someone's activities between 2 and 9 days ago. This is an approximation based on the more complex model used by the Risk Tracker, which is based on the following sources:
-
Ferretti et al shows that transmission to someone else within 2 days of getting infected is very unlikely.
-
McAloon et al gives us a distribution of how long it takes for a person to develop symptoms:
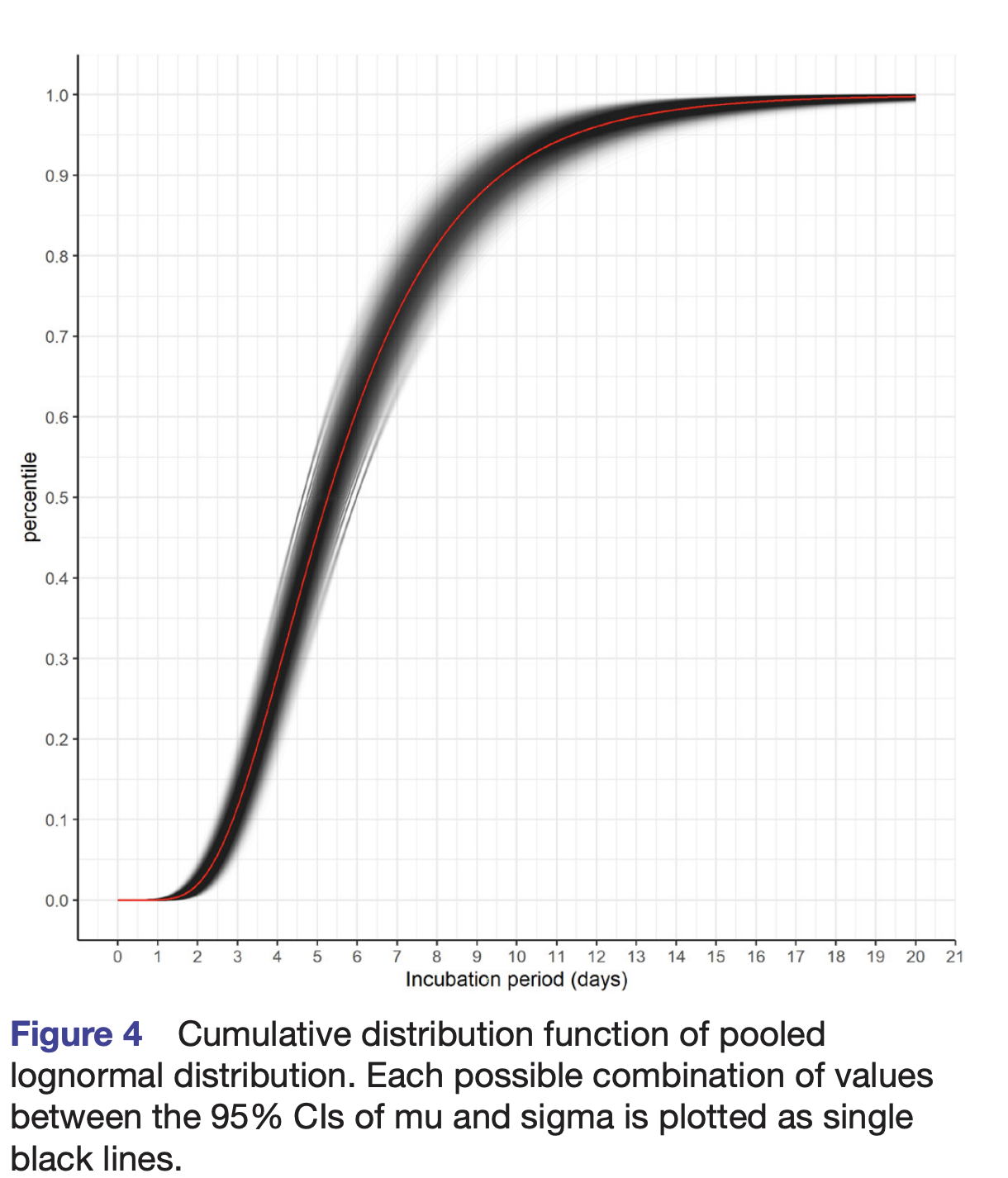
-
Byambasuren et al tells us that 17% of COVID cases never develop symptoms and these cases are 42% as likely to transmit COVID to others compared to patients who have or will develop symptoms.
-
Covid Strategy Calculator gives us a distribution for probability of infection conditioned on not having symptoms, which we combine with McAloon et al. to derive a lognormal distribution for risk of never symptomatic cases.
-
Lee et al. Shows that 50% of cases that are never symptomatic are completely recovered (undetectable amounts of virus) in 16 days and 90% are recovered in 23 days.
Combining these sources, we built a model that accounts for time to developing symptoms, proportion of cases that are asymptomatic, and decreased infectiousness of asymptomatic individuals:
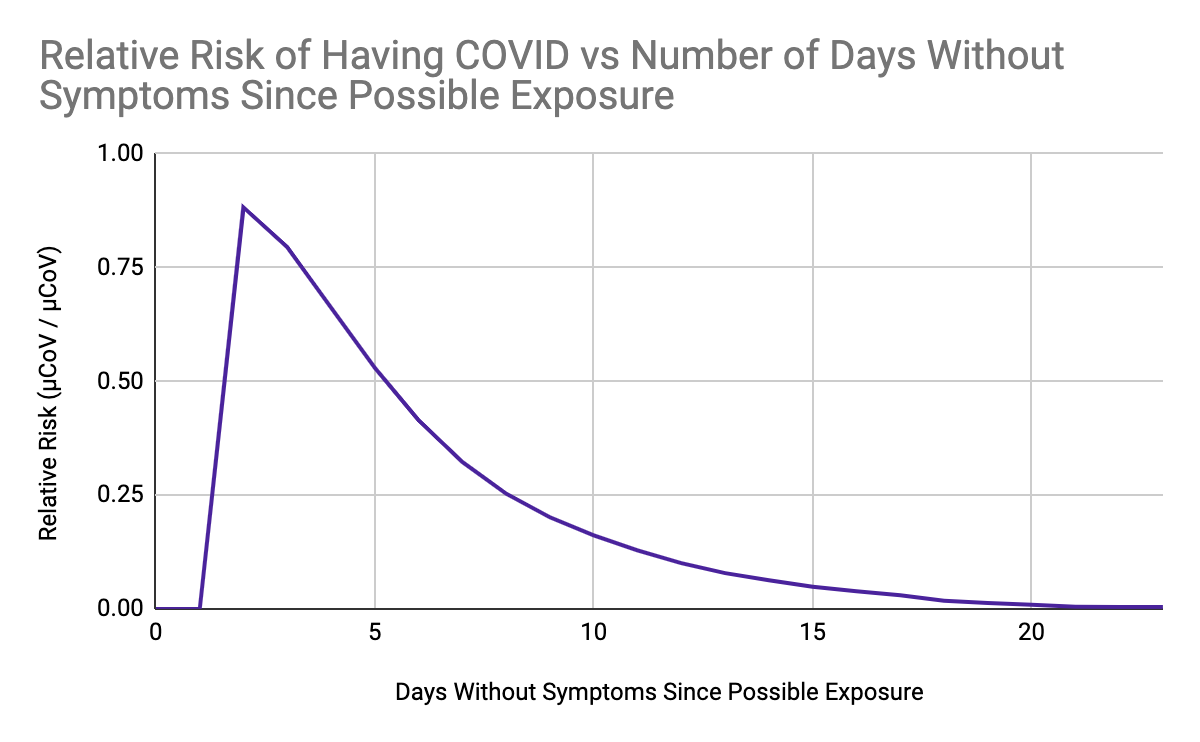
This peaks on day 2 and decays over time. Since the risk starting around day 20 is small, we arbitrarily choose a cutoff time of 23 days, which yields an infectious window of exactly 3 weeks (2-23 days).
Many people have a weekly routine, which makes modeling their risk for 7 days compelling. If a person regularly gets a total of X microCOVIDs over the course of 7 days and they do the same activities each week, then learning they are currently symptom-free allows us to estimate their current risk of having COVID as 60% lower than their weekly total X.
Explaining how we calculate that: they will have done the activity exactly 3 times in any past 2-23 day window so we can estimate that their risk on any given day will be:
3 * X * SUM(Relative Risk) / 21 days = 0.6 * X
Therefore a person with a regular schedule could be modeled based on their normal 7 day week, but users tracking risk with the Risk Tracker will be able to more precisely know the risk they pose to others on any given day.
The 2-9 day window cited elsewhere in the whitepaper is one way of simplifying this decay over time, by treating it as though there is no decay from day 2 through 9, and then all the decay occurs as a sharp step on day 10. This is purely a simplification: there is absolutely nothing magical about day 9; in reality, on day 10 there is still 16% of the original risk left. If a person’s risky activities do not follow a 7 day cycle, and they have some something very risky more than 9 days ago, you may need to ask them for what they have done for up to the last 2 or even 3 weeks.
Note on Infectious Period: Contacts' symptoms
Another important thing to know about the infectious period is that only about 9% of transmissions from people who eventually show symptoms occur more than 3 days before those symptoms appear, and only 1% occur more than 5 days before symptoms appear. We get this data from He et al, Figure 1c middle graph:[4]
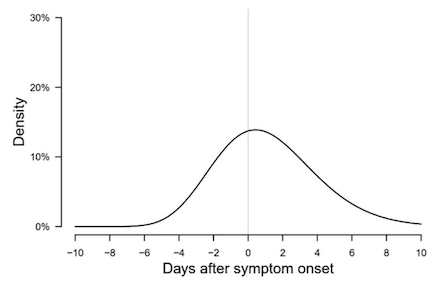
One insight we can gain is that since 50% of transmission occurrs after symptoms onset, if you confirm with the person you are seeing that they don't have symptoms right before you interact, you are reducing your risk by 50%.
Additionally, only about 6% of transmissions come from people who won't ever show symptoms (Ferretti et al):[5]
These two facts combined imply that, if you interacted with someone more than 3 days ago, and that person has not yet shown symptoms, then you should be about 7 times more confident than you were before that they did not transmit COVID to you: 0.94*0.09 + 0.06 = 0.14 ≈ 1/7.
And if your interaction was 5 days ago and your contact still has no symptoms, you should have an additional 2x as much certainty (total of 14 times more confident): 0.94*0.01 + 0.06 = 0.07 ≈ 1/14.
To see where these factors might be useful in practice, imagine that Alice lives with risk-averse housemates but wishes to spend undistanced time with her partner Bob, who generally acts in riskier ways. Without further information, Alice might imagine that she needs to isolate for 10 days after spending time with Bob in order to avoid exposing her housemates to more risk than they're comfortable with. But suppose seeing Bob is the only high-risk thing Alice is doing, and suppose that Alice and her housemates have modelled Bob using the Advanced Method and all agree that he is only 5x "too risky." (That is, if Bob were 5x less likely to have COVID at the time of Alice's visit, Alice's housemates would be fine with Alice seeing Bob and then coming back home without further isolation.) Then Alice could safely follow a procedure where she:
- has her visit with Bob;
- waits 3 full days without interacting with Bob or her housemates;
- verifies that Bob is not experiencing any potential symptoms of COVID-19, even mild or ambiguous ones;
- and then returns home.
This works because Bob is less than 7x "too risky." If he were 10x "too risky," Alice could safely wait 5 days instead of 3, because 10x is less than the 14x increased confidence that you can have after 5 days.
If each visit only requires 3 or 5 days of isolation instead of 10, Alice can probably see her partner more often, which is likely to be good for both Alice's and Bob's mental health.
Vaccines
Assumptions
- We use Byambasuren et al. as our source for transmission from asymptomatic cases; they found that (in an unvaccinated population), 17% of cases never have symptoms and these individuals are 42% as likely to transmit COVID as individuals who eventually have symptoms.
- From this we calculate that for every infection, there are .83 symptomatic infections and .17 never-symptomatic infections.
- Or, for every symptomatic infection, there are .17 / .83 ≈ .2 asymptomatic infections (we use this extensively below)
- We assume that individuals who are tested once per week with a PCR test and never test positive are not infectious to others. This is not a perfect, as PCR tests have a non-trivial false negative rate, but we presume that the false negative rates in control and trial groups cancel out.
Delta Variant Revision Note
We are in the process of updating the data / calculations below with data for vaccine performance against the Delta variant. We used the following sources:
- Bernal et al. studied vaccine efficacy for Pfizer and and AstraZeneca's vaccine:
“after 1 dose of vaccine with B.1.617.2 cases 33.5% (95%CI: 20.6 to 44.3) compared to B.1.1.7 cases 51.1% (95%CI: 47.3 to 54.7) with similar results for both vaccines. With BNT162b2 2 dose effectiveness reduced from 93.4% (95%CI: 90.4 to 95.5) with B.1.1.7 to 87.9% (95%CI: 78.2 to 93.2) with B.1.617.2. With ChAdOx1 2 dose effectiveness reduced from 66.1% (95% CI: 54.0 to 75.0) with B.1.1.7 to 59.8% (95%CI: 28.9 to 77.3) with B.1.617.2."
- Edara et al. showed similar antibody neutralizing rates between Pfizer and Moderna's vaccines, leading us to (continue to) use the same numbers for Pfizer and Moderna.
- We were unable to find data on vaccine effectiveness vs. never-symptomatic infection with the Delta variant. We used applied the same ratio of symptomatic to asymptomatic infections per vaccine as found previously (see below for sources for each vaccine).
- We were unable to find data on Johnson&Johnson's vaccine vs the Delta variant. We combined the following:
- Johnson & Johnson's phase 3 study included data for subtrials in South Africa in which 95% of cases were the Beta variant. They found that vaccine efficacy against moderate to severe-critical COVID-19 was 64% in this subtrial.
- Tada et al. found that the Beta and Delta variants had similar levels of antibody neutralization, roughly suggesting that the two variants have similar propensity for immune escape.
- Thus, we used efficacy from the South African arm of Johnson & Johnson's vaccine trials as the efficacy of the vaccine vs. the Delta variant.
AstraZeneca
AstraZeneca’s trial used at-home test kits to test for asymptomatic cases of COVID. Their study reported that, among fully vaccinated participants, there were 57 never-symptomatic cases and 84 symptomatic cases, or .68 never-symptomatic cases per symptomatic case.
Bernal et al. found a 59.8% (95%CI: 28.9 to 77.3) reduction in cases of symptomatic COVID among people fully vaccinated with AstraZeneca's vaccine.
For each symptomatic case among unvaccinated people, this gives us:
| Control Group | Vaccinated Group | |
|---|---|---|
| Symptomatic Cases | 1 | .4 |
| Never symptomatic cases | 0.2 (Byambasuren) | .4*.68 = .27 |
Treating never-symptomatic cases as .4 relative infectiousness, this gives an infectiousness adjusted ratio of:
(.4 + .4 * .27) / (1 + .4 * .2) = 0.47
Moderna & Pfizer
Phase III trials from Moderna and Pfizer (the most common vaccines in the United States) both found 95% reductions in symptomatic COVID cases.
The CDC released a study showing 90% reduction in all cases (symptomatic + asymptomatic) 14+ days after participants received Moderna or Pfizer’s vaccine.
We then back-calculate the number of asymptomatic cases among vaccinated individuals:
- For every symptomatic case among unvaccinated people, there are .2 unsympomatic cases, or 1.2 total cases (Byambasuren)
- For every symptomatic case among unvaccinated people, there are .05 symptomatic cases among vaccinated (Phase III studies)
- For every total case among unvaccinated people, there are .1 total cases among vaccinated people (CDC)
- For every symptomatic case among unvaccinated people, there are 1.2 * .1 = .12 total cases. (1 & 3)
- For every symptomatic case among unvaccinated people, there are .12 - .05 = 0.07 asymptomatic cases among vaccinated people. (2 & 4)
- For every symptomatic case among vaccinated people, there are 0.07 / 0.05 = 1.4 symptomatic cases among vaccinated people (2 & 5)
We then combine this with Bernal et al. which found Pfizer's vaccine to be 87.9% (95%CI: 78.2 to 93.2) effective at reducing the chance of symptomatic infection by the Delta variant.
| Control Group | Vaccinated Group | |
|---|---|---|
| Symptomatic cases | 1 | .12 (Bernal) |
| Never symptomatic | .2 (Byambasuren) | .12 * 1.4 = .17 |
Treating never-symptomatic cases as .4 relative infectiousness, this gives an infectiousness adjusted ratio of:
(.12 + .4 * .17) / (1 + .4 * .2) = 0.17
We assume that Pfizer’s vaccine has similar performance as Moderna’s on the basis that they have similar designs and reported metrics.
Additionally, a study of the Pfizer vaccine in the UK of 23,324 participants found 86% reduction of symptomatic and never-symptomatic cases. Israel’s study of 500,000 vaccinated individuals suggests 92% reduction in all cases of COVID-19, but we have some concerns over the completeness of their coverage of never-symptomatic cases.
Israel’s study provides much more complete data on the risk reduction for severe COVID (the Phase III studies for both Moderna and Pfizer were underpowered to determine this). They found a 92% risk reduction for severe COVID among participants who had received both doses of the Pfizer vaccine. Note that “severe illness” is defined by NIH as requiring supplemental oxygen (i.e. hospitalization).
Johnson & Johnson
For Johnson & Johnson’s vaccine, we used data from a brief filed with the FDA based on their Phase III study. The J&J trial tracked both symptomatic and never-symptomatic infections. Johnson and Johnson performed serology assays for non-spike-protein antibodies on days 1, 29 and 71 to track never-symptomatic infections. They also counted an never-symptomatic infection if a participant presented with a positive PCR test but no symptoms. Symptomatic cases were counted if a patient presented with symptoms and tested positive via PCR at least 14 days after administration of the vaccine.
| Control Group | Vaccinated Group | |
|---|---|---|
| Symptomatic Cases (14-71 days) | 351 / 19544 | 117/19514 |
| Never-symptomatic Cases (0-29 days) | 182 / 19809 | 159 / 19739 |
| Never-symptomatic Cases (29-71 days) | 54 / 19162 | 22 / 19301 |
From this data we get a ratio of rougly .18 asymptomatic cases per symptomatic case.
We are currently unable to find research of Johnson & Johnson's vaccine's effectiveness vs the Delta variant. In lieu of data for Delta variant:
- Tada et al. found that the Beta and Delta variants had similar levels of antibody neutralization, roughly suggesting that the two variants have similar propensity for immune escape.
- Johnson & Johnson's phase 3 study included data for subtrials in South Africa in which 95% of cases were the Beta variant. They found that vaccine efficacy against moderate to severe-critical COVID-19 was 64% in this subtrial.
Therefore we provide the efficacy of the vaccine against the Beta variant, with the expectation that this is similar to the efficacy against the Delta variant.
| Control Group | Vaccinated Group | |
|---|---|---|
| Symptomatic cases | 1 | .36 (J&J Phase 3, South Africa arm) |
| Never symptomatic | .2 (Byambasuren) | .36 * .18 = .065 |
Treating never-symptomatic cases as .4 relative infectiousness, this gives an infectiousness adjusted ratio of:
(.36 + .4 * .065) / (1 + .4 * .2) = 0.36
We note that Johnson & Johnson reported significantly more never-symptomatic cases in days 0-29 of the trial compared to 29-71. Rather than complicate the calculator by adding a slightly higher second number for the first 29 days, we suggest simply noting this and being more cautious during days 14-29 while your immunity is still increasing.
Sputnik V (Gamelaya Research)
Not yet updated for the Delta variant
The efficacy of the Sputnik V vaccine produced by the Gamelaya Research Institute is based on their phase 3 trial information published in Lancet. Our calculation is similar to the one used for Moderna & Pfizer. Non-symptomatic cases were not measured in this study, so based on Byambasuren et al. and the CDC study about Moderna/Pfizer, we estimate non-symptomatic cases to be 17% of all cases in the control group and 50% in the vaccinated one. As the control and the vaccinated group had a different size, we also have to normalize the adjusted infectiousness figures.
This is how the numbers look like 14 days after dose 1:
| Control Group | Vaccinated Group | |
|---|---|---|
| Participants | 4,950 | 14,999 |
| Symptomatic Cases | 79 | 30 |
| Never symptomatic cases | 16 (0.17 / (1-0.17) x symptomatic cases) | 30 (= symptomatic cases) |
Now we can calculate the overall effect on contagiousness:
- Control group adjusted contagiousness =
(79 * 1 + 16 * .42) / 4,950 = 1.73% - Vaccinated group adjusted contagiousness =
(30 * 1 + 30 * .42) / 14,999 = 0.28% - Relative contagiousness of vaccinated group =
0.22 / 1.73 = 0.16.
This is how the numbers look like 7 days after dose 2:
| Control Group | Vaccinated Group | |
|---|---|---|
| Participants | 4,601 | 14,094 |
| Symptomatic Cases | 47 | 13 |
| Never symptomatic cases | 10 (0.17 / (1-0.17) x symptomatic cases) | 13 (= symptomatic cases) |
Now we can calculate the overall effect on contagiousness:
- Control group adjusted contagiousness =
(47 * 1 + 10 * .42) / 4,601 = 1.11% - Vaccinated group adjusted contagiousness =
(13 * 1 + 13 * .42) / 14,094 = 0.13% - Relative contagiousness of vaccinated group =
0.10 / 1.11 = 0.12.
The trial also measured efficacy 21 days after dose 1, on the day of dose 2, with practically equivalent numbers to what they saw 7 days after. This suggests that the Sputnik V vaccine offers a strong protection 2-3 weeks after the first dose, and the second dose is only required for long-term protection.
Single Shot Efficacy
For a single dose of vaccines require 2 doses, we used Bernal et al. which reported 33.5% efficacy vs symptomatic COVID for a single dose of either Pfizer and AstraZeneca's vaccines.
Moderna provided a supplement from their Phase III trial that suggested .6 asymptomatic infections per symptom infection 3 weeks after the first dose.
| Control Group | Single Dose Vaccinated | |
|---|---|---|
| Symptomatic | 1 | 0.665 (Bernal et al.) |
| Asymptomatic (subtract) | .2 (ratio from Byambasuren) | 0.4 (0.6 x symptomatic) |
This gives an overall multiplier of (0.665 + .4 * .4) / (1 + .4 * .2) = 0.76 for Moderna, Pfizer, and AstraZeneca.
Others' Vaccines
For the purposes of providing an estimate of the riskiness of an "average vaccinated person", we must consider that the "average" person in a region has some likelihood of being vaccinated. A vaccinated individual is (vaccine multiplier) times less likely to get COVID than the average unvaccinated individual, which is not the same as the average individual.
We make the assumption that vaccinated and unvaccinated people are doing roughly the same activities - we explicitly don't like this assumption, but don't have good data for what ratio of risky activites to use instead.
Then:
Average prevalence = sum(prevalence in group * proportion of population in group)
= sum(vaccine_mult * unvaccinated_prev * proportion of population)
Unvaccinated risk / Average risk = sum(vaccine_mult * proportion of pop)
= population / sum(vaccine_mult * proportion of pop)
Where the sum is taken over all vaccine types and status (including no vaccine)
To get data for vaccine prevalence, we use data from JHU for Countires and US States, combined with data from Covid Act Now for vaccines in a county. JHU breaks down vaccinations by manufacturer for US States, and we assume that US Counties have the same ratio of vaccine types.
We do not have a data source for vaccine type breakdown in countries outside the US; we calculate as if all vaccines were AstraZeneca. This results in under-estimating the riskiness of unvaccinated people and over-estimating the riskiness of vaccinated people in countries where more effective vaccines are being used.
We have not (yet) done this calculation for other risk profiles; the calculation is somewhat different. The Risk Tracker remains the best tool for estimating the risk of a vaccinated person whose behaviors are known.
48% came from taking the previous household transmission figure 30% and multiplying by 1.6x (we had not factored in the Lewis et al. paper at time of calculation). ↩︎
We find it easier to understand the difference between an odds ratio and a risk ratio in a medical context. If 100 people walk into your clinic with heart disease, and twice as many were smokers as non-smokers, then the odds ratio is 2x. But that doesn’t tell you what you would get if you started with 50 smokers and 50 nonsmokers and watched for heart disease later. You don’t know what the base rate of smoking was in your original dataset. See https://psychscenehub.com/psychpedia/odds-ratio-2 for more on this. ↩︎
We understand there’s currently somewhat of a debate or discussion around whether COVID is best thought of as being transmitted by smaller droplets that can linger in the air, or mostly by larger droplets that fall down quickly due to gravity. We already thought the evidence was pointing towards lingering droplets, and Prof. Jimenez’s writeup on the topic summarizes this perspective far better than we could. ↩︎
If you were previously familiar with this source, note that it was substantially updated in a 07 Aug 2020 author correction. ↩︎
There's an inconsistency in Ferretti et al, where the main text states that total transmissions come "10% from asymptomatic individuals (who never show symptoms), and 6% from environmentally mediated transmission via contamination.", whereas Figure 1 and Table 2 report the reverse, 6% from asymptomatic and 10% from environmental. We choose to go with the Figure 1 and Table 2 estimates. ↩︎
Uncertainty Estimation
Warning: the entire uncertainty estimation section needs to be revisited for the Delta variant. Proceed with caution.
In this writeup, we've presented individual numbers for all the parameters of our model:
- 30% Activity Risk from a housemate per week, or 48% from a partner
- 6% baseline Activity Risk per hour (indoor, unmasked, undistanced)
- Various multiplicative risk reductions (2x per 3 feet (1 meter), 2x for your mask, 4x for their mask, 20x for outdoors, etc)
- Person Risk underreporting factors of 6x/8x/10x depending on positive test rate
Based on the sources we've described so far, we think these numbers are the best estimate of the truth — that's why we're presenting them instead of some other numbers. But of course there's still a lot of uncertainty about the details of COVID transmission, which means that it's possible, even likely, that some or all of the numbers we're using will turn out to be off by a little or a lot. In this section, we attempt to answer the question: "if we're wrong, how wrong might we be?".
The top-line answer: we think the numbers produced by our calculator are correct within a factor of 10, and probably within a factor of 3. That is, if the calculator says some activity has a risk of 300 microCOVIDs, the risk might well actually be 100 or 1000 microCOVIDs. (And the calculator will tell you that, alongside the result it gives you.) It could be as few as 30 or as many as 3000 microCOVIDs, but that would be a lot more surprising to us.
The rest of this section explains how we came up with those bounds, and will be much more jargon-heavy.
We estimated underlying probability distributions for a subset of the parameters in our model: the protection factors for masks, distance, and outdoors, the baseline Activity Risk of 6%, and the underreporting factor for prevalence. In some of these cases, we were able to do this estimation using the confidence intervals that were reported in the scientific papers that we used as sources. In other cases, our sources did not provide clear confidence intervals, so we had to resort to fuzzier intuition. We then combined these distributions using Monte Carlo simulation to produce distributions for the risk of three example activities, and compared these to the calculator outputs.
We did this analysis using Guesstimate, an online tool that makes it easy to do math on probability distributions. (Imagine a spreadsheet where each cell is a random variable instead of just a number.) Our work is spread across two Guesstimate models:
- Masks and distance data (using uncertainties from published sources)
- Overall model (using uncertainties from the masks-and-distance model and from the authors' current beliefs)
In the following subsections, we go into more detail on the rationale behind the distributions in the Guesstimate models. When we say "A (B to C)", we mean we think a random variable is distributed with median A and 90% confidence interval B to C. We have represented 95% confidence intervals in our sources as 90% confidence intervals in the Guesstimate models, because Guesstimate is designed to work with 90% confidence intervals and we figure the extra uncertainty doesn't hurt.
Masks
Note: This analysis has not been updated to use the new sources from the Jan 2021 masks update.
Wearer protection: We use Chu et al as the source for our wearer protection data in this model. This study directly measured reduction in coronavirus infections (SARS, MERS, and COVID-19) as a result of mask wearing and other measures. We conservatively use the smaller risk reduction that they report for non-healthcare settings: someone wearing a surgical mask has 0.56x (0.41x to 0.80x, lognormal) the risk of infection as someone not wearing a mask. The studies in this group were all for SARS. Taking the reciprocal of this, we find the mask provides 1.7x (1.2x to 2.5x, approximately lognormal) protection. (Our other sources are more optimistic than Chu about the benefit of masks, so it seems sufficiently conservative to only include Chu.)
Protection to others: We use the following two studies to estimate uncertainty:
- From Milton et al., surgical masks reduced exhaled influenza virus count by 3.3x (1.8x to 6.3x, lognormal).
- From Fischer et al, we take droplet counts that were produced in different trials by the same speaker when speaking through the four different cotton masks that were tested, as well as no mask. Averaging the droplet counts through the four cotton masks and dividing by the droplet count with no mask, we find a 5.3x (2.9x to 8.7x) reduction. We acknowledge that droplet count is not the same as virus count which is not the same as risk of infection, but we think the one is a reasonable proxy for the other.
- Averaging these two estimates, we get a source control factor of 4.4x (2.9x to 6.7x).
Note: we also cite Davies et al. as a data source, but they do not state clear error bounds.
Distance
We limit our analysis to the decrease in risk specifically between one meter and two meters of distance. We find:
- From Chu et al, a risk reduction factor of 2.1x (1.1x to 3.8x). (Chu reports this per meter: from "no distance" (which we think is probably more like half a meter than zero) to one meter, and from one meter to two meters.)
- From Hu et al. (the train passenger study), we compare attack rates for two different scenarios.
- In one, we compare "same row two seats away" (1 or 1.1 meters distance) to "same row four seats away" (2.1 meters distance). We find that the further distance is associated with a 4.3x (2.1x to 10x) reduction in risk.
- In another, we compare "one row and one column away" (1.02 meters distance, by the Pythagorean theorem since rows are 0.9 meters apart and columns are 0.5 meters apart) with "one row and three columns away" (1.74 meters distance). ("Column" here refers to the number of seats away in the direction perpendicular to the direction the passengers are facing.) We used three columns away rather than four columns away, even though four columns was closer to 2 meters, because the attack rate for one-row-four-columns seemed uncharacteristically low (lower than five columns away) and it would have artificially inflated our estimate of the protection factor from greater distance. We find that the further distance among this pair is associated with a 2.9x (0.9x to 10x) reduction in risk.
- Averaging the estimate from Chu with the average of the estimates from Hu, we get a 3.0x (1.9x to 4.9x, approximately lognormal) reduction in risk when going from one meter to two meters.
Remaining parameters
These are in the main Guesstimate sheet, not the sub-sheet that was used for the mask and distance data, because we're no longer able to base our distributions on the confidence intervals from our sources: the remaining parameters come from sources without obviously usable confidence intervals. We don't have fully legible justifications for the intervals that we've chosen; they're derived from our intuitions based on reading papers and listening to statements by public health officials for a few months. If you want to see the impact of different choices, you can edit the Guesstimate model. (Don't worry, it won't change what anyone else sees.)
- Reduction in risk from being outdoors: 28x (9x to 95x), computed by combining the following guesses:
- Transmission due to breathing and speaking might be reduced by 10x to 100x, lognormal (implies a median of 31x, mean 40x).
- Transmission due to coughing and sneezing (which happen even in people who would describe themselves as healthy) is probably only reduced 1x to 3x, lognormal (median and mean about 2x).
- Overall transmission from people who don't know they're sick might be 90% due to breathing and speaking, and only 10% from sneezing and coughing, because even though sneezing and coughing are much more effective at transmitting the virus, people who feel well usually don't sneeze and cough very much.
- Baseline transmission risk (indoor unmasked 1-hour conversation at typical socializing distance, point estimate 6%): 2% to 13%, lognormal (median 5%, mean 6%).
- Underreporting factor in San Francisco (point estimate 6x): 3x to 10x, lognormal (median 5.5x, mean 5.9x).
Results
Now that we have all the above distributions, we can multiply them together for typical scenarios, and compare the results against what we get using the calculator.
- Outdoor hangout (
prevalence ⨉ baseline / outdoors): calculator says 12 μCoV, uncertainty-based model says 1.5 to 36 μCoV (mean 10, median 6). - Indoor masked hangout (
prevalence ⨉ baseline / (my mask ⨉ their mask)): calculator says 30 μCoV, uncertainty-based model says 7.7 to 92 μCoV (mean 32, median 24). - Indoor unmasked hangout (
prevalence ⨉ baseline): calculator says 236 μCoV, uncertainty-based model says 67 to 640 μCoV (mean 230, median 179).
We note the following:
-
The calculator result is quite close to the mean of the underlying distribution of the uncertainty-based model. Taking into account all of the information available to us, that means we think we're neither overestimating nor underestimating on average (i.e., low or no bias).
-
Multiplying the calculator result by 3 yields in each case a value that is close to or above the upper end of the 90% confidence interval from the model. Dividing the calculator result by 3 yields a value that is somewhere between 1.2x and 2.6x higher than the lower end of the 90% confidence interval from the model. For ease of communication, we'll call that a 3x margin of error in either direction. We think we might be overestimating by a greater factor than we might be underestimating, but that's the direction we'd prefer to err in if we must — no disaster will befall if some action turns out to be safer than we told our users it might be.
Note: This analysis is about known unknowns, i.e., places where we know there's uncertainty and can reasonably estimate how much. We have not characterized the uncertainty in all parameters of the model; we have only demonstrated that, under some typical scenarios, the uncertainty might be low enough to make the results usable. Additionally, it is entirely possible that there is more uncertainty beyond what we've calculated here, due to some unforeseen problem in our (individual or society-wide) understanding of COVID transmission dynamics. At the beginning of this section we quoted bounds of 10x, not 3x; this discrepancy is intended as a hedge against such "unknown unknowns", but we have no way of knowing if it's enough. Use our model with care.
Calculator Changelog
1/4/2022: Omicron variant vaccine updates
Made first-round updates for Omicron.
- Vaccines
- Efficacy of vaccines vs any infection has greatlly decreased.
- Added the option to have a booster dose.
- Pfizer / AstraZenica data was drawn from Ferguson et al., Table 3.
- Pfizer multiplier changed to 1, 0.8, 0.25 with 1, 2, or 3 doses respectively.
- AstraZenica changed to 1, 1, 0.3.
- Moderna / Sputnik is assumed to be similar
- Johnson&Johnson data is from Gray et al., calculated from data in table 1 as (Number of positive COVID19 tests With Vaccine / Number of tests With Vaccine) / (Number of positive COVID19 tests without Vaccine / Number of tests)
- New multipliers are 1, 0.95 with 1 or 2 doses.
- To handle mixed-vaccines, we are only looking at the most recent dose. This is a simplification to make the UI and research manageable. In reality, e.g J&J followed by Moderna is probably a little worse than 2 Modernas while Moderna followed by J&J is probably a little better than 2 J&J’s.
- We acknowledge that vaccine efficacy decays over time. We will attempt to add this to the model in the near future.
- Other mutlipliers
- We do not think Omicron affects the housemate or partner multipliers.
- Lyngse et al found that the secondary attack rate within households of unvaccinated individuals was nearly identical between Omicron and Delta.
- We therefore suspect that Omicron also does not affect the hourly multiplier, but do not have data for this.
- If you have contact tracing data that suggests a new hourly transmission rate, please send it our way.
- We do not think Omicron affects the housemate or partner multipliers.
7/26/2021: Delta variant updates
- Updated transmission and vaccine numbers for Delta variant:
Previous Delta Variant Hourly Multiplier 9% 14% Housemate 30% 40% Partner 48% 60% J&J .34 .36 AstraZeneca .4 .47 AstraZeneca Single Dose .56 0.76 Pfizer/Moderna .1 0.17 Pfizer/Moderna Single .56 0.76 - See blog post or Research Sources for more details.
6/22/2021: Add "Average vaccinated person" risk profiles
- Added the option to select the vaccination state of average people
- Imported vaccination data from JHU and Covid Act Now.
- See Research Sources for derivation and caveats.
5/27/2021
- Updated constants for under-reporting factor
- New numbers from COVID 19 Projections December 2020 update.
- Results in slightly lower prevalence estimates.
4/10/2021
- Added Gamelaya Research's Sputnik V vaccine to the calculator. See the Research Sources section of the White Paper for details.
3/30/2021: Add Johnson & Johnson's vaccine
- Vaccine updates:
- Added support for Johnson & Johnson's vaccine (single dose, 1/3 multiplier).
- Improved multiplier for Moderna and Pfizer's vaccines (0.2 -> 0.1) based on new data.
- Increase wait time before getting the effects of a vaccine (7 -> 14 days). This matches Moderna / AstraZeneca / Johnson & Johnson (Pfizer's was the only study that used 7 days).
- See Research Sources for rationale.
3/16/2021: Add vaccines to Risk Tracker
- The latest version of the Risk Tracker now supports modeling the risk of someone you are seeing who is vaccinated.
2/21/2021
- Added precaution for being vaccinated. See paper Q&A and Research Sources for details.
- Note: vaccines also reduce the risk of people who you interact with, we just haven't implemented this yet.
2/2/2021
- Remove "frontline worker", "healthcare worker", and "works from home" person risk categories.
- Remove the "Intermediate Method" from the white paper. You can read more about our rationale for this change.
1/28/2021
- Created new mask categories and updated multipliers for mask types. See the Masks section of Research Sources in the White Paper for details.
1/5/2021
- Increased One-time interraction transmission rate from 6% to 9% to account for more contagious COVID variant B117. See blog post for details.
1/2/2021
- Re-labeled "frontline worker" to "healthcare + social worker".
- Reduced risk of healthcare + social workers to 2x average (previously 3x).
- Re-labeled "Not an essential or front-line worker" to "a person who works from home."
- Note This recategorizes people who work outside the home but not in healthcare/social work settings as "An average person in your area."
12/19/2020
- Fixed a bug in which many counties were getting the state's positive test ratio instead of the counties.
- Updated to COVID Act Now's v2 API, allowing positive test rates to sync again.
12/13/2020
- Replaced logic for under-reporting factor, resulting in significantly lower prevalence estimations.
- Previous logic: 6x for positive test rate under 5%, 8x for 5%-15%, 10x for above 15%.
- New logic from COVID 19 Projections
- See Research Sources for more details.